Rapamycin
The most powerful tool to stop the acceleration of aging caused by mTOR dysfunction and cellular senescence.
The "Hallmarks of Aging" represent a crucial turning point in the scientific understanding of the aging process. These hallmarks, first articulated in a landmark 2013 paper and recently expanded, capture the key physiological and molecular shifts that occur as we age. In this two-part article, we'll delve into these revised hallmarks, focusing first on the 'Primary Hallmarks,' and the age-related pathways they affect. To begin, we will start with the “Primary Hallmarks” of aging: Telomere Attrition, Genomic Instability, Epigenetic Alterations, Loss of Proteostasis, and Disabled Macroautophagy.
rapamycin
metformin
16 mins
By: Jacob Rose
The scientific field of aging is in an interesting place because even though aging and its manipulation have been discussed for thousands of years, it has only been directly interrogated for just over 100 years. Indeed, in the early 1900s scientists started to record lifespan curves and set out on the epic quest to slow or stop this philosophical inevitability.
If we fast forward about a century, we find that scientists have made incredible process in developing tools to answer questions about aging, and know certainly a lot of the things that cause it, but are still struggling to put all the pieces together. Realizing the incredible overlap and mosaicism in aging, a group attempted to put all these pieces in a neat, concise publication called The Hallmarks of Aging.
The Hallmarks of Aging (2013) was an immediately successful review published in Cell, because it gave an exhaustive take on all the well-studied phenomena that are known to contribute to aging. This landmark paper specifically features a graphic with all the hallmarks in a circle that every aging scientist has seen in introduction PowerPoint slides.
This graphic is especially prolific because it allows the presenter to smoothly highlight the hallmark they intend to address in their work. Since 2013 people have adopted one or more of these hallmarks as the cornerstone of their work, attempting to mitigate aging by repairing or circumventing alterations in them.
10 years later, the same authors got together and updated their work to fit into a field that saw a decade of improvements and named it “An Expanding Universe”. In their update, they took the original nine hallmarks, reassessed them, and decided that there were significant clarifications and divisions that needed to be addressed and added three more hallmarks, totaling 12. Another improvement to the original paper includes further delineation of these hallmarks into Primary, Integrative, or Antagonistic drivers of aging.
Primary drivers of aging are more or less thought to be the “source” of aging because their presence alone is sufficient to induce an aging phenotype. These primary drivers of aging are the tips of the aging iceberg, if you cause genomic instability, you cause age-related disease and are actively contributing to the appearance of the integrative and antagonistic hallmarks.
Even though the authors painstakingly make these neat boxes to put certain hallmarks into, by grouping them in this way, they address the interconnectivity of aging phenotypes. Each of these hallmarks, primary or otherwise, have biological mechanisms and molecular pathways that are dysregulated and are known to cause age-related disease. The major goal of this two-part article is to outline these hallmarks and the pathways that become dysregulated with age within each hallmark. To begin, we will start with the “Primary Hallmarks” of aging: Telomere Attrition, Genomic Instability, Epigenetic Alterations, Loss of Proteostasis, and Disabled Macroautophagy.
Telomere Attrition, or Telomere Shortening, has been an attractive phenomenon to study for a long time because of telomere’s obvious protective role in gene quality. Imagine you are building an incredibly long bridge with a finite amount of “bricks”. You lay the bricks one at a time and because you haven’t built too many sections of bridge with your cache of bricks you have plenty to finish the section and plenty in excess to stand on as you finish one section of the bridge. As you start adding sections, you realize (after 60 or 70 years of bridge building) that your excess bricks are dwindling quickly, so much so that you may be caught at the very edge of a bridge with no excess bricks to stand on.
Our telomeres are the extra bricks that our genetic machinery stand on as they finish replicating the DNA in our chromosomes. As we age, this brick storage dwindles and leaves very little room for our genetic machinery to sit and function properly. As such, the machinery building genetic bridges begin making mistakes, and cutting off sections of the actual bridge instead of excess.
Additionally, in the case of our genetic material, these short, loose ends cause the genetic material to fray, unwinding the double helix in important sections of the chromosome and, more often, exposing them to stress they would otherwise be protected from.
So, are there ways to air-drop more genetic bricks? Probably soon, but there are a few things to very heavily consider. Telomeres are also important as quality control measures for cell genome health. If the cell’s telomeres are short, a cell has likely divided many times over and therefore is likely to accumulate genetic damage along the way, increasing the risk of a cell becoming cancerous.
Short telomeres act as early warning signs for innate anti-cancer mechanisms (one specifically covered in the Antagonistic Hallmarks) and are sufficient to put these cascades in action. The balancing act lies in keeping our genome healthy long enough to divide more (build more bridges) without the risk of cancer developing.
Countless labs have laid the groundwork for therapeutic companies to attack this delicate problem. Telomerases are enzymes that would be able to airdrop telomeric repeats, or genetic bricks, to critically shortened genes.
Targeted treatments with telomerase are becoming more attractive as we narrow down on which genes they should protect, allowing us to reinforce the most important parts of our genome without increasing the risk of cancer. Speaking of cancer and genetic complications! The next hallmark we will interrogate is Genomic Instability.
Our chromosomes are made up of tightly bound DNA and this tightly bound DNA must be unraveled to fit all the molecules required to express the subset of genes that form chromosomes. When a gene is expressed at a high level, the protein it encodes is generated more often. Controlling gene expression is second nature to cells, and many things can either promote or restrict gene expression, thereby controlling the proteins created in response to the cellular environment.
Genomic instability comes in many forms, is caused by various stressors, and typically results in aberrant cell death or cancer initiation. Genotoxic agents are incredibly relevant to our everyday life and in contemporary news, certain artificial sweeteners have been found to have genotoxic effects. Other common genotoxic agents are used clinically as chemotherapies, like cisplatin and doxorubicin. Radiation exposure, either in radiotherapy or in a typical sunburn, are also common stressors on the gene environment.
These stressors are especially dangerous because they efficiently cause double-stranded DNA breaks and limit the capacity of the DNA damage response (DDR) to fix the damage. If the DNA is damaged beyond the capabilities of the DDR, the cell undergoes programmed cell death (apoptosis) to prevent damaged genes from being replicated. Low-level, chronic genomic stress accumulates with age and the sliding scale of an individual’s mutation burden and DNA repair capabilities will determine if the cells become cancerous.
The most obvious example of this is cancer caused by excessive sunburns. People who do not wear sun protection are at a higher risk of skin cancers; the sustained, low-level exposure to UV rays causes breaks in the genome, and, depending on both your inherited mutations and DDR capabilities, is dealt with by repairing the DNA or initiating apoptosis cascades causing cell death and subsequent skin peeling. If the would-be cancer is able to fly under the radar long enough by having mutations in key tumor-prevention genes, it will likely become cancerous and need to be removed through extrinsic cell activity or human intervention, which are unsurprisingly affected by other aging hallmarks.
“Genomic instability may be the single most integrated hallmark of aging and as such, the possibilities and complications attached to addressing it are equally as puzzling.”
There are therapeutics that interact with the DDR, but many currently available drugs are most applicable in cancer and cause particularly strong off target effects because their specificity for the cancer is rather low.
To complicate matters further, some cancers have subsets of functional DDR machinery, while some are mutated and dysfunctional. Mutations in the BRCA1/2 genes are commonly known to predispose women to breast and ovarian cancer. These mutations cause a dysfunction in the arm of DDR machinery designed to link pieces of broken DNA.
Knowing this, it is possible to inhibit another DDR enzyme, called PARP1, to completely block cancer DDR and cause the cancer to accumulate an unescapable amount of DNA damage. It is plain to see that these drugs are not suitable for preventative use, and drugs designed to passively bolster genome health aren’t available at this time.
However, one way to involve yourself with your genome is to sequence yourself! Products and services like 23 and me can give very valuable information about your genes and the mutations you have. I would also encourage anyone who wants more information to see a genetic counselor. These are trained professionals that will guide you through your chromosomes and pinpoint where your genes are generating the most risk. Certain versions of genes will put you at risk for age related diseases or as I described above, certain cancers.
In my old life, I was able to see that I have a single copy of APOE4, a deleterious version of APOE, which puts me at elevated risk for neurodegeneration and Alzheimer’s disease. However, now that I know that about myself, I can put more efforts into mitigating cognitive decline as I get older.
Another great opportunity to see a genetic counselor is when you are interested in having children. Sequencing both parents is a great way to check for unfavorable mutations that may lead to genetic diseases like Huntington’s.
Even though there aren’t currently magic preventative therapies to bolster genome health, there are ways to interact with your genes and use the information to make meaningful decisions about your health. Another way to assess your age is to measure the epigenetic alterations made to your genes!
Now that we are well versed in your genes, let’s take it a step further. More involved readers may have heard of Epigenetic Clocks before, and may have even given blood with the intent to measure their “epigenetic age”.
Epigenetics is the study of the modifications to DNA that affect a certain gene’s behavior and expression. These modifications come in many flavors, but for aging, the most important thing to track is DNA methylation. Epigenetics is of particular interest because it is another way that our lifestyles and exposures interact with our genes. When we are exposed to a stress, we want our genes to express the blueprints for the tools to deal with it, and, as a result, the tightly bound DNA of our chromosomes unwind so they may be expressed. Epigenetic modifications make this pattern more robust, allowing easy access to genes that need to be expressed more often.
Methyl “writers” add methyl groups, and “erasers” remove them, there are also enzymes known as “readers” that help guide the enzymes into proper function, but for the purpose of this article, we will be speaking more generally about how these methylation profiles correlate with age. How specific modifications can affect certain genes is still under study and is highly context-dependent, but in general, a DNA methylation profile will provide striking clues to biological and chronological age.
In 2013, a scientist named Steve Horvath created what is now known as the “Horvath Clock”. Steve Horvath and his team took many different tissues and cell types, mapped their DNA methylation patterns, and discovered that these methylation profiles were not only similar between tissues and cell types, but were also tightly tied to the age of the tissue.
Even when scrutinized by the field and more samples were tested, the Horvath Clock faithfully predicted chronological age. To this day, it is still under incredible dispute what the clock is actually measuring and how it works so well, but if you’re interested in how your “epigenetic age” matches up to your real age, I would encourage you to look up commercially available clocks and send a sample in. This finding has really opened the door for more people to design their own clocks, which all measure slightly different things, but in general, return similar results.
Now that your crash course in genes and genetics is over, it’s time to move on to slightly bigger (literally and figuratively) concepts.
As a protein expert, I would argue that proteins are the most important biological molecule in our body. As biased as that statement is, there is a protein for every function our cells need to perform. Need structural integrity? Proteins. Need to move things around? Proteins. Need to transcribe genes? Proteins. Need to catalyze the breakdown of food, toxins, or other foreign material? Proteins. This wonderful, pervasive fact is also why there is an entire hallmark of aging dedicated to their dysregulation.
The loss of proteostasis refers to the idea that the normal steady state of all the proteins in our body can go awry. If homeostasis is the steady state of our body or a specific system, then proteostasis is the equivalent of proteins.
Something fascinating about proteins is their 3D structure. Plenty of biologists think about sequences in a vacuum, genes have DNA sequences, proteins have amino acid sequences, but they forget that these sequences also exist in a world where shape and orientation matter. Imagine the relationship of a lock and key, if the key isn’t the correct width, height, or depth, it does not matter how perfectly the teeth align with the lock.
Similarly, if the lock doesn’t have a sturdy house for the key, the relationship fails. Proteins are very similar to this and their proper function is tightly regulated by their shape and their shape is regulated by the interplay of their environment with their sequence.
If a protein is created, but there is a mutation in the genes that encode the protein, the sequence changes, and therefore, the function changes. There are numerous diseases attributed to this phenomenon and some are on their way to being treatable by fixing the problem with the original gene.
Short-term treatments usually involve giving patients functional versions of the protein they cannot correctly generate, called enzyme replacement therapy. Additionally, if the environment a protein is working in is abnormal, the function of that protein can change, alterations in temperature or cellular pH are common causes of protein misfunction.
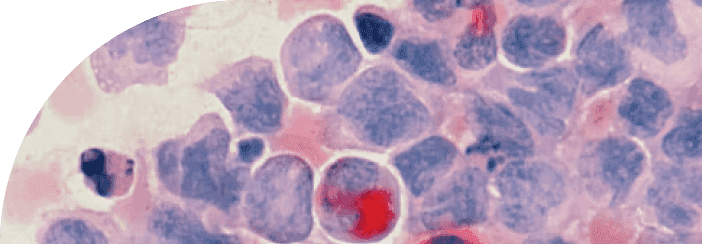
What happens if a cell recognizes that a protein isn’t shaped correctly? You guessed it, proteins take care of it. This class of proteins is called chaperones and they are responsible for refolding proteins that are misshapen. If the protein is irreparably misfolded, another protein tags it so a different protein will come to degrade it and recycle its amino acids for energy or to make new proteins. The most famous example of the loss of proteostasis is the aggregation of neurotoxic protein bundles during neurodegeneration.
Tau and Amyloid beta are two specific proteins that are known to aggregate in the brains of people who experience a wide array of neurodegenerative diseases. More involved readers will already know that treatments removing amyloid plaques are not efficacious putting some labs back at square one. The relationship between amyloid beta aggregates and neurodegeneration clearly needs more interrogation, but the tenets of clearing them using pharmaceuticals are still valuable. We know that these drugs will function as intended by solubilizing aggregated amyloid beta, and hopefully in the future drugs to combat the loss of proteostasis will be more effective at alleviating disease.
Tau is still an interesting target and is known to be responsible for the generation of “tauopathies” or diseases that are caused by the presence of insoluble tau tangles, but it won’t be a surprise to say that more work needs to be done to understand the role of pathogenic tau and amyloid beta. Dealing with these aggregates also falls under the purview of the next hallmark, and if your cells need to deal with entire ecosystems of proteins in one fell swoop, we need to talk about disabled macroautophagy.
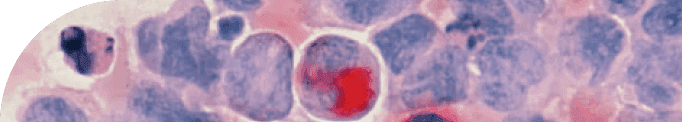
Rounding out the primary hallmarks is disabled macroautophagy which is just a fancy term for large scale (in the cellular context) recycling of cellular material. Until now, the hallmarks have been relatively small changes that make large contributions to aging. When talking about autophagy, we are increasing the scale quite a lot. Instead of single genes, modifications, or proteins, we are discussing a large group of those individual components cohesively dealing with a toxic, or unnecessary member of the cellular environment.
The most important player in this cellular function is a lysosome. Lysosomes are small, acidic vesicles that serve as a garbage disposal for unsavory or otherwise dysfunction things that enter our cells. You may be able to imagine that the buildup of trash and nonfunctional organelles can wreak havoc on the cellular environment. Those poor proteins won’t have a chance to hold their shape!
Major, inherent dysfunction of the lysosome causes a family of diseases called Lysosomal storage diseases or LSDs. Treatment options for people with LSDs are similar to the ones described above, replace the dysfunctional enzyme as often as needed, or create a gene therapy that corrects the error. “However, as with all the hallmarks, it is not only the catastrophic failure of autophagy machinery that can contribute to aging, small perturbations are also able to have cumulative, deleterious effects.”
Luckily, of all the hallmarks in this article, altering macroautophagy has been very well studied in reference to one pharmaceutical that is known to bolster this key function. Rapamycin’s main function is to inhibit the mTOR pathway. However, mTOR function also has a very strong anti-autophagy response and thereby inhibiting it, will increase autophagy.
Inhibiting mTOR has also shown benefits not relating to autophagy, but we will tackle those relevant hallmarks in the next article. Other drugs like metformin have also been shown to improve autophagy, but we are learning that context is always incredibly important. One of these drugs may be more applicable under certain conditions, in certain organ systems, or in diseases than the others.
Improving autophagy has clear benefits, especially when applied to the toxic protein aggregates described in the Loss of Proteostasis section. Modulating the ways our cells deal with garbage has incredible potential to slow age-related disease, and as more details surrounding lysosomes and their related machinery is uncovered, more specific and effective drugs can be used.
Thus, concludes the first five hallmarks of aging. The other seven hallmarks are more similar to disabled macroautophagy in that they involve entire cellular systems, not just singular genes or proteins. It is important to appreciate, however, that even the tiniest changes to the most basic parts of our cells and bodies will initiate crucial cascades that conclude with huge implications. Each of the hallmarks are opportunities for us to interact with aging, understand how it is driven and, if we are committed and educated, how to slow it.
TAKE HOME POINTS
The hallmarks of aging is an incredible pair of papers that concisely describe what is known about aging and what causes it.
Each of the hallmarks represents opportunities for scientists and the public to interact with aging biology.
The primary hallmarks start small, with the building blocks of our cellular processes and expand into much larger, functional compartments of organelles.
Even in cases where preventative medications or supplements aren’t readily available, it is possible to interact with your health and hallmarks in meaningful ways.
Citations
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.