.png?u=https%3A%2F%2Fimages.ctfassets.net%2Fzvzqa1d1gh0f%2F68YrPbjn5g7t8jFrx2OLuQ%2Fb206487615608c4585c6e309d8dd9567%2Flabs_2__1_.png&a=w%3D55%26h%3D55%26fm%3Dpng%26q%3D75&cd=2025-06-12T20%3A31%3A13.529Z)
Metabolic Pro Panel
Assess key biomarkers (A1C, Insulin, hsCRP) to detect imbalances and guide interventions that boost longevity & energy.
For decades, muscle loss was viewed as an inevitable byproduct of aging—an aesthetic concern or athletic obstacle. But emerging research reveals a deeper truth: skeletal muscle is a central regulator of aging, capable of influencing inflammation, metabolism, and even the clearance of dysfunctional, senescent cells. In this Research Review, Dr. Richard LaFountain, Healthspan’s Senior Scientist, explores how resistance training functions as a molecular intervention—stimulating immune responses, enhancing mitochondrial health, and reducing the burden of cellular senescence in both muscle and fat tissue. Drawing from recent preclinical and human studies, he also introduces the concept of backcasting: a strategy for planning present-day strength goals to preserve physical function decades into the future. The message is clear—regardless of age, resistance training offers one of the most powerful tools we have to extend not just lifespan, but strengthspan.
Muscle Mass
mitochondrial health
Biomarkers
Anti-Inflammation
Cellular Senescence
25 mins
By: Dr. Richard LaFountain
Aging is inevitable, but how we age is not. One of the most powerful tools for shaping that trajectory is resistance exercise. Far beyond aesthetics or sport, lifting weights and moving with intention turns on molecular pathways that counteract the biological drivers of aging, particularly the accumulation of dysfunctional, “zombie-like” senescent cells. These cells contribute to chronic inflammation, impaired regeneration, and the gradual erosion of strength, resilience, and independence.
Importantly, decline is not linear. Strength, power, and cellular function deteriorate faster with age, especially in the absence of sufficient physiological reserve. This makes long-term planning essential. Backcasting, a framework popularized in the longevity field by Dr. Peter Attia, offers a practical way to do this. You begin with a future goal: for example, lifting a 50-pound bag of soil at age 90. Then, using known rates of decline, you work backward to determine the strength you’ll need today—potentially a 230-pound deadlift in your 30s—to retain that capacity decades later. Without this intentional overshoot, many individuals fall below clinical thresholds for mobility and independence as senescence and frailty accelerate.
Resistance training uniquely supports this strategy. It builds muscle and bone, enhances metabolic flexibility, and reduces systemic inflammation, all while activating signaling pathways that suppress or eliminate senescent cells in muscle, adipose tissue, and beyond.
In this review, Dr. Richard LaFountain, Healthspan’s Senior Scientist, provides a scientific and practical framework for understanding how resistance training influences cellular aging. Readers will gain insight into how to backcast effectively, structure training with aging trajectories in mind, and incorporate resistance exercise as a cornerstone intervention to preserve strengthspan, delay frailty, and extend healthspan.
To understand how resistance training combats aging, we first need to understand what drives aging at the cellular level. Aging isn’t simply the passage of time—it’s the biological wear and tear that erodes the body’s ability to repair itself. Over time, cells lose their regenerative edge, accumulate damage, and become metabolically sluggish. The result is a slow but steady breakdown of function across nearly every system in the body. [1,2]
One of the most pivotal mechanisms in this process is cellular senescence [1]. When a cell becomes too damaged to safely divide—whether due to oxidative stress, DNA damage, or shortened telomeres—it doesn’t immediately die. Instead, it enters a state of suspended animation. These cells, often referred to as “zombie cells,” are neither alive in a useful sense nor completely dead. Originally, this state served a protective function, helping prevent runaway cell division and cancer. But over time, the balance shifts. As senescent cells accumulate, they begin to act like saboteurs from within. As more of proportion of cells in a tissue become senescent, the organ begins to experience a decline in function.
What makes these cells so destructive is their secretory profile—known scientifically as the senescence-associated secretory phenotype, or SASP [3,4]. This cellular cocktail contains inflammatory cytokines, enzymes, and other signaling molecules that disrupt surrounding tissue and, alarmingly, coax neighboring cells into senescence as well. It’s a biological chain reaction—one that accelerates tissue dysfunction, fuels chronic inflammation, and contributes to many hallmark diseases of aging, including sarcopenia (muscle wasting), cardiovascular disease, and insulin resistance.
In a healthy body, the immune system acts as a cleanup crew, identifying and removing senescent cells to maintain tissue integrity. But as we age, this internal surveillance falters—a phenomenon known as immunosenescence.
While the immune system typically clears senescent cells, its efficiency declines with age [5], leading to a buildup of these dysfunctional cells. First described in the early 2000s, immunosenescence refers to the gradual decline in immune system function that accompanies aging [5]. Surprisingly, this process may begin much earlier in life than we realize. The thymus, the organ responsible for producing new T cells (the body’s foot soldiers in immune defense), starts to shrink and lose function soon after childhood [6]. A noticeable decline in immune system function accelerates considerably after the 4th or 5th decade of life, such that by age 60, new T cells are no longer created. [6,7].
The consequences of this immune decline ripple far beyond increased infection risk. A weakened immune system also struggles to clear senescent cells, allowing them to persist and spread [8]. This breakdown in immune regulation helps explain why autoimmune diseases like rheumatoid arthritis, systemic lupus erythematosus (SLE), and multiple sclerosis (MS) are often associated with signs of accelerated aging [9,10,11]. In rheumatoid arthritis, for instance, patients exhibit early thymic dysfunction, increased T cell aging, and widespread inflammation—traits typically seen in much older individuals. These patients also face higher rates of age-linked diseases such as osteoporosis, cardiovascular disease, and even neurodegenerative conditions.
Fortunately, this story is not one of inevitable decline. Emerging research shows that lifestyle interventions, including changes to diet, movement, and microbiome health, can significantly delay or even reverse aspects of both cellular senescence and immunosenescence [11,12,13]. Multiple systematic reviews now point to nutrition and exercise as two of the most effective strategies. These interventions have been shown to reduce inflammatory cytokines such as IL-6 and IL-7, modulate DNA methylation patterns, and enhance immune resilience. Among these tools, resistance training stands out—not only for building muscle and strength but also for its ability to function as a therapeutic ally in managing age-related and autoimmune conditions.
Let’s review the research on the magnitude of the effects of resistance training on the levels of cellular senescence and analyze the mechanisms by which it delivers its benefits.
Senotherapeutics are agents or interventions known to improve how the body manages cellular senescence. This growing category of interventions falls under the umbrella of senotherapeutics—agents or strategies that target the burden of cellular senescence. Broadly, senotherapeutics are divided into two classes [13,14,15]:
Senolytics - pharmacological agents that selectively eliminate senescent cells
Senomorphics - molecules that target and suppress the senescence-associated secretory phenotype (SASP) in senescent cells, without inducing cell death
Recently, greater attention has been directed toward lifestyle interventions that produce senotherapeutic effects, including exercise, nutrition, sleep, probiotics, and even hormetic stressors like cold or heat [11,16,17]. Lifestyle interventions, or habits, can be deployed or stacked as an integrated strategy to reduce an inevitable accumulation of senescence, thereby delaying the less desirable consequences of aging.
Preclinical research is leading the charge, offering compelling evidence from animal models that exercise can have senotherapeutic effects, preventing senescence and reducing the number of senescent cells in various organs, including the heart, liver, muscles, kidneys, and adipose tissue [18]. For example, mouse studies suggest that aerobic exercise in the form of wheel running or swimming reduces markers of senescence:
In the heart, aerobic exercise has been shown to lower expression of p16, a cyclin-dependent kinase inhibitor that serves as a key marker of senescence.
In the kidneys, it reduces beta-galactosidase activity—another hallmark of aged or damaged cells.
In the liver, exercise suppresses proinflammatory cytokines like interleukin-6 (IL-6), helping to quiet the destructive signaling associated with SASP.
These effects suggest that exercise seems to be reducing the overall burden of senescent cells in the tissue itself—this has important implications for the extension of healthspan. What began as a promising insight from animal studies is now being echoed in human research: cellular senescence is not just measurable—it’s modifiable.
Scientists have identified a growing list of biomarkers that reflect senescent cell burden in the human body. These markers span molecular, functional, and even clinical domains, offering a multi-dimensional window into how we age and how our biology responds to interventions. [22,23,24]. One of the most well-established indicators is p16^INK4a, a protein whose expression rises with age and cellular damage. Notably, p16 levels appear to be independent of gender or body mass index, but they are highly responsive to lifestyle inputs—particularly physical activity and intermittent fasting (in the range of 17–19 hours) [25,26]
A growing body of human data now supports the role of exercise as a potent intervention to lower the burden of senescent cells.
One particularly compelling study, published in 2023, compared master athletes—adults in their late 50s who consistently engage in endurance training—with two other groups: sedentary peers of the same age, and a younger control group (average age 24). The results were striking: the master athletes had senescence markers nearly identical to those of the younger adults, while the sedentary 57-year-olds showed almost double the levels of p16 and interleukin-6 (IL-6) in their colon mucosa compared to both active and young participants [28].
These findings highlight a crucial point: exercise appears to slow, or even partially reverse, molecular hallmarks of aging in tissues well beyond muscle. Research from multiple groups has now demonstrated improvements in senescence markers across various cell types, including adipose tissue [27], endothelial cells [29], and even gut epithelium [28]—a testament to the systemic reach of physical activity as a cellular therapy.
Several research groups have published data supporting senescence biomarker improvement following exercise training in various cells and tissues, including adipose tissue [27], colon mucosa [28], and endothelial cells [29]. This data adds another dimension to the longevity benefits associated with exercise.
Among all the tissues in the body, skeletal muscle plays a uniquely central role in how we age. Skeletal muscle is crucial to maintaining metabolic health, physical function, and independence. And as we grow older, maintaining muscle health becomes one of the most powerful ways to preserve both function and longevity.
Yet aging brings an almost universal decline in muscle mass and quality. This process, known as sarcopenia, reflects more than just shrinking biceps or diminished strength—it signals a deeper deterioration in the cellular health of muscle tissue. Increasingly, researchers have found that cellular senescence is intimately linked with muscle atrophy [31,32]. As senescent cells accumulate within skeletal muscle, they create a proinflammatory environment that disrupts tissue repair, impairs mitochondrial function, and accelerates metabolic dysfunction [33].
In this light, muscle can no longer be seen merely as a mechanical structure—it is increasingly recognized as a pivotal organ of longevity [34,35,36]. Muscle isn’t just affected by aging; it also shapes how we age.
When muscle health declines, the effects cascade through the body. Senescent cells in muscle not only degrade local tissue, they also contribute to systemic inflammation and metabolic instability. This makes it harder for the body to regulate blood glucose, lipid metabolism, and energy balance—functions that are essential for maintaining metabolic flexibility. And when metabolic health falters, the risk of chronic disease rises sharply.
Indeed, poor muscle health has been associated with higher rates of age-related diseases, including cardiovascular disease, certain cancers, type 2 diabetes, and neurodegenerative disorders like Alzheimer’s and Parkinson’s disease [37]. These conditions often share common roots in chronic inflammation and impaired energy regulation—both of which can be influenced by the health and cellular environment of skeletal muscle.
Maintaining healthy muscle mass is essential for healthy cellular function and reducing senescent cell accumulation, aging, and chronic disease risk. Skeletal muscle acts as a biological buffer against the aging process, both structurally and metabolically. But what’s less well known is that muscle also plays the role of a communication hub, actively influencing distant organs and cellular systems through biochemical signaling.
In fact, skeletal muscle is one of the largest endocrine organs in the body. When muscles contract—especially during regular exercise—they release a vast array of signaling molecules known as myokines. To date, researchers have cataloged more than 3,000 different myokines, many of which have far-reaching effects on inflammation, metabolism, tissue regeneration, and cellular aging [38,39].
These myokines function like molecular messengers, some sending stimulatory signals that enhance repair and energy metabolism, others exerting inhibitory effects that dampen inflammation or prevent excess tissue growth. When muscles are regularly activated through movement or resistance training, they release a cascade of anti-inflammatory and anti-senescent myokines that benefit not just the muscles themselves, but the entire body.
Myokine Effects Summary
Figure 1. Muscle action during movement and exercise stimulates the release of myokines that have distributed effects and anti-aging benefits throughout the body.
One of the most intriguing discoveries in this area is irisin, a myokine that is directly induced by physical activity [39]. Irisin has been shown to exert senotherapeutic effects—it supports mitochondrial function, reduces oxidative stress, and helps tissues remain metabolically youthful [39]. Its discovery helped solidify the idea that muscle isn’t just reacting to aging—it’s capable of sending out signals that actively slow it.
Other key myokines also show promise in this regard:
Growth differentiation factor-15 (GDF-15) and fibroblast growth factor-21 (FGF-21) have been linked to enhanced fatty acid oxidation, lipolysis, and improved energy metabolism.
Interleukin-6 (IL-6)—typically seen as a proinflammatory cytokine—can act as an anti-inflammatory myokine when released in the context of exercise.
Myostatin, a regulator of muscle growth, helps calibrate tissue remodeling and may influence the balance between regeneration and senescence.
While we typically think of cytokines in the context of inflammatory signaling—often contributing to the accumulation of senescent cells—this particular subset of myokines acts in the opposite direction. They are anti-inflammatory, and, in many cases, help to reduce the overall senescent burden. In this context, activating muscle contractions becomes not only a mechanical act of movement, but a molecular intervention against aging.
Our bodies reach their peak muscle and bone mass in early adulthood—typically between the ages of 20 and 30. After that, decline begins quietly, often imperceptibly at first. From age 30 onward, most individuals lose about 1% of muscle and bone mass per year [40]. After age 50, this process accelerates, with strength losses climbing to 1.5–5% annually [41]. The cumulative effect is striking: while skeletal muscle makes up roughly 50% of total body weight in young adults, this proportion can fall to just 25% by age 70 or 80 [48].
Accumulation of excess senescent cells plays a causal role in driving this muscle tissue aging process and aggravates sarcopenia pathology, which may initiate chronic disease progression [42].
Compounding the issue is the selective loss of type II (fast-twitch) muscle fibers, which are essential for strength, power, balance, and independence. These fibers decline even more rapidly than total muscle mass—at rates of up to 3% per year beginning in early adulthood, particularly in individuals who are not regularly engaging in resistance training [40]. One reason for this is denervation: as muscles remain unused, they lose neural connections, making it harder to generate force and respond to the physical demands of everyday life.
The effect of inactivity is profound—and fast. In older adults, just 10 days of bed rest due to illness or injury can lead to a 10% or greater loss in strength and functional capacity [43]. Over time, the nervous system also suffers. By age 70, most individuals have lost up to 40% of their motor units, the fundamental units that allow muscles and nerves to work together [44].
This cascade—muscle loss, denervation, and declining function—is a major driver of frailty, osteoporosis, impaired immune function, and reduced lifespan [40,45].
The factors that accelerate muscle loss with age are not solely biological—they’re deeply influenced by lifestyle. A sedentary routine, low-quality nutrition, and lack of resistance training all contribute to an environment that favors cellular deterioration. These behaviors not only shrink muscle mass over time but also impair the function of muscle stem cells—the very cells responsible for regenerating and maintaining muscle tissue [42].
As stem cell activity wanes, the body’s ability to rebuild and repair muscle becomes compromised, leading to progressive losses in strength, power, and mobility. What begins as subtle weakness can evolve into sarcopenia, frailty, and reduced independence. But this trajectory isn’t fixed—it’s modifiable.
The timing of intervention matters. Incorporating resistance training early in life, particularly in late adolescence or young adulthood, yields outsized benefits. This is the window during which the body can build up what researchers call a “physiological reserve”—a surplus of muscle strength, bone density, and regenerative capacity that serves as a buffer against future decline [35,36]. Much like saving for retirement, this reserve can be drawn upon later in life, helping individuals maintain function as the natural aging process progresses.
Crucially, regular strength training doesn’t just build tissue—it sends a powerful molecular signal to the body to resist senescence. It helps preserve muscle stem cell function, limits the accumulation of senescent cells, and suppresses the proinflammatory SASP signals that contribute to tissue breakdown and systemic aging [42].
Put simply, resistance training is a biological countermeasure. The earlier it's adopted, the more profound its protective effects—not just for muscle health, but for aging itself.
Regular exercise, particularly resistance training, is one of the most effective interventions for preserving muscle and bone mass throughout lifespan. When we engage in weight-bearing movements or exercises that apply force to the skeleton, we stimulate osteoblasts—the bone-building cells responsible for maintaining bone density and structure [45]. At the same time, both mechanical and chemical stress from strength training promote muscle mass and strength increase by activating motor unit nerves [44], creating mild damage in muscle, which is repaired and improved during recovery [34, 35, 36].
This process—known as adaptive remodeling—is how muscle becomes stronger. TThese adaptations involve more than just changes in muscle fibers. In addition to building strength and supporting skeletal integrity, resistance training drives powerful cellular adaptations. It enhances mitochondrial function, the efficiency and density of the tiny power plants inside our cells that generate energy. Healthier mitochondria translate to better cellular performance across tissues—from muscles and fat to the brain and cardiovascular system [46].
Resistance exercise also improves insulin sensitivity, making it easier for the body to regulate blood sugar and store nutrients efficiently—key defenses against metabolic diseases like type 2 diabetes. Just as importantly, it lowers systemic inflammation, helping to quiet the chronic, low-grade inflammatory signals that are increasingly recognized as a hallmark of aging.
Together, these three effects—on mitochondria, insulin signaling, and inflammation—form a triad of protection for cellular health, reinforcing the idea that resistance training is not just about mobility or aesthetics, but a core strategy for slowing the aging process at the cellular level.
Crucially, it’s never too late to start. While early adoption of strength-building habits offers the greatest long-term protection, research shows that even older adults—those with advanced muscle loss or diagnosed sarcopenia—can regain significant strength and mass through properly structured resistance training [35,46,47]. The myth of irreversible decline is steadily being replaced by a more hopeful truth: skeletal muscle remains highly adaptable throughout life.
In fact, muscle is one of the most regenerative tissues in the human body. It exhibits remarkable plasticity, with an estimated cellular turnover rate of ~1.5% per day [48]. Unlike many organs that accumulate damage without adequate self-repair, muscle has a built-in ability to heal, remodel, and even grow stronger after injury or stress—especially when that stress comes in the form of intentional training [49]. This regenerative potential makes muscle a unique lever in the pursuit of longevity.
Understanding that resistance training can slow aging at the cellular level is one thing—knowing how to do it effectively is another. Fortunately, evidence-based guidelines offer a clear starting point for those looking to preserve muscle mass, strength, and function across the lifespan.
Current recommendations suggest engaging in resistance training 2 to 3 times per week, with each session lasting between 20 and 60 minutes—adding up to roughly 1 to 3 hours per week [35]. Within that modest time commitment lies enormous potential to build strength, maintain independence, and slow key drivers of biological aging.
But it’s not just about showing up at the gym. To effectively counteract sarcopenia, resistance training should include dynamic movements that activate all major muscle groups through both concentric (lifting) and eccentric (lowering) muscle actions [50]. These movements are essential for stimulating both strength and muscular control, which are critical for maintaining balance, mobility, and functional independence with age.
Equally important is the quality of effort. Building muscle and enhancing strength requires attention to training volume (sets and reps), load (weight or resistance), and intensity (how close to fatigue each set is performed). This is where the concept of progressive overload becomes vital.
Progressive overload refers to the gradual increase in resistance or difficulty over time. By consistently challenging muscles with slightly greater demands—more weight, more reps, or less rest—the body is signaled to adapt. This adaptive stress is what drives muscle growth, neuromuscular improvements, and the beneficial molecular responses associated with resistance training.
Muscle Mass and Strength Across Lifespan
Figure 2. Muscle Mass and Strength Across Lifespan. Consistent, safe, resistance training will produce the greatest peak at a later age, which improves trajectory in avoiding physical limitations to healthy movement as well as reducing the risk of clinical frailty or disability.
Meaningful gains in muscle mass and strength often require training at a moderate to high intensity. Specifically, exercising at or above 70% of one’s one-repetition maximum (1-RM)—the maximum weight a person can lift for a single repetition—is typically necessary to generate the biological signals that promote muscle growth [47,50].
Meta-analysis data suggest 20.5 weeks of consistent resistance training produced a significant 2.4 lb or 1.1 kg increase in lean body mass in aging men and women [51]. This addition of muscle mass is especially significant in the context of the high prevalence of sarcopenia. Estimates are that half of all 80-year-olds may be classified as sarcopenic [52]. Building healthy muscle mass can simultaneously attenuate sarcopenia risk and reduce the impact of cellular senescence and chronic disease by increasing strengthspan [53].
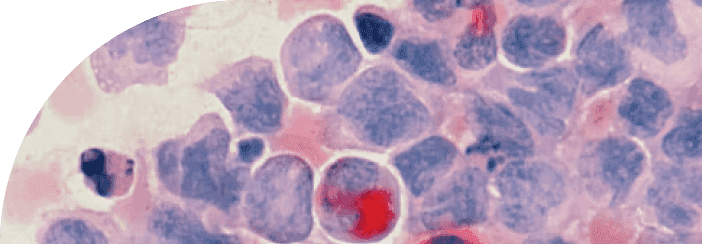
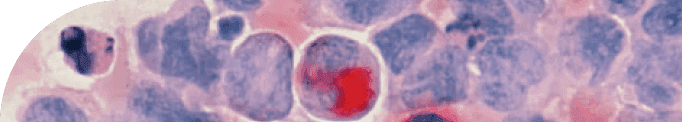
Research published in 2018 by Yang et al. examined changes of p16(INK4a) positive senescent cells in skeletal muscle before, immediately following, and 48 hours after a single bout of resistance exercise with multiple biopsies in college-aged males [54]. In the experiment, participants also consumed either a low-protein (14%) or high-protein (44%) supplement prior to the workout. The exercise protocol consisted of six sets of 12 squats at 70% of 1-repetition max (1-RM)—a stimulus sufficient to stress the muscle and trigger recovery processes [54].
Following the workout, there was a dramatic surge in immune activity within the muscle tissue: leukocyte infiltration increased by 82% to 230% depending on the protein condition [54]. Leukocytes identify damaged tissue, clear cellular debris, and target dysfunctional or senescent cells for removal. In this study, their increased presence suggests that resistance exercise triggers an acute inflammatory response that mobilizes immune surveillance in muscle. Interestingly, those in the low-protein group showed a greater spike in leukocyte activity, suggesting that lower protein intake may heighten the acute inflammatory response that draws immune cells to the site of tissue disruption. Most notably, nearly 50% of p16^INK4a-positive senescent cells were cleared from muscle tissue immediately following the workout [54].
Interestingly, the same research team included a 12-week resistance training program following the aforementioned acute experiment. The resistance was set at 70% of each participant's 1-RM for both the high and low protein groups. Each session consisted of 3 sets, 12 repetitions (70% of 1RM), 3 times per week [54]. The training load was increased by 20% with the same set and rep scheme at the beginning of week 5 for all participants [54]. At the conclusion of 12 weeks, muscle mass increased to a greater extent (+1.08 kg) in the high protein group, whereas the low protein group added less muscle mass (+0.40 kg) [54].
Lower protein supplementation may improve senescent cell clearance following acute resistance exercise. However, higher protein intake offers greater benefits in building muscle mass alongside consistent training. According to these data, senescent cell clearance is enhanced by lower protein intake coupled with resistance exercise, which stimulates inflammation and brings immune cells to affected muscle tissue to commence repair and rebuilding [55]. Based on these data, cycling protein intake may offer hybrid benefits. Pairing acute resistance exercise with lower protein intake may produce more acute senescent cell clearance, while consistent resistance training in conjunction with high protein intake increases muscle mass growth.
Another study published in 2018 by researchers at the Sticht Center for Healthy Aging and Alzheimer’s Prevention included a 5-month resistance training intervention study that significantly reduced senescent cell abundance [27].
In this study, participants with an average age of 72 years and a BMI of 30 kg/m² completed a 5-month resistance training program, exercising three days per week. At the end of the intervention, biopsies from thigh adipose tissue revealed a 60% reduction in p16^INK4a-positive senescent cells—from 5.47% at baseline to just 2.17% post-training [27]. This significant drop highlights the responsiveness of even non-muscle tissues—like fat—to the molecular effects of resistance exercise.
Taken together, these results provide compelling evidence that both acute resistance exercise and consistent training can produce dramatic reductions in cellular senescence markers, across tissue types and across lifespan. In 2018, two separate lab groups published data demonstrating dramatic reductions in p16(INK4a) positive senescent cells. This was shown in the adipose tissue [27] and muscle tissue [54] of females and males spanning ages 22 to 72 in response to guided resistance exercise training programs.
Regardless of age, investing effort and time in exercise, especially resistance training, produces global benefits to health while improving quality of life through increases in healthy muscle mass.
Backcasting is a strategic planning method popularized in the health and longevity space by Dr. Peter Attia. It involves “reverse engineering” long-term goals by starting with a desired future outcome and working backward to determine the steps needed to achieve it. While the concept has gained recent traction in personal health, it has long been used in complex business and policy planning to improve long-range outcomes [56,57].
In a health context, backcasting begins with a vision of the physical capabilities, lifestyle quality, and experiences you want to maintain in future years or decades. From this idealized future, you work backward to identify what actions must be taken today—especially regarding your physical health—to make that vision a reality. When it comes to strength and mobility, it’s essential to acknowledge a biological truth: muscle mass, strength, and power will inevitably decline with age, despite our best efforts [40,46,48]. The key, then, is to build a surplus—a physiological reserve—that exceeds your immediate needs. Overshooting your target now creates a buffer against the inevitable losses to come.
This concept mirrors the logic of retirement planning. Most people save more than the bare minimum to account for uncertainty and the declining purchasing power of money over time. One of the worst-case scenarios in retirement is outliving your savings.
Similarly, maintaining physical reserves well above the threshold for daily function provides insurance against aging-related losses. Individuals who only meet the minimum strength required for independence face a much greater risk of crossing below clinical thresholds for sarcopenia, osteoporosis, frailty, and loss of autonomy. Unfortunately, many people are on track to outlive their physical health reserves—even if they have ample financial savings. Without sufficient muscle mass and functional capacity, their long-term goals and envisioned lifestyles may go unrealized due to limitations in the physical health required to enjoy them.
This proactive approach is critical because the decline in muscle mass, strength, and cellular health is often non-linear. While physical deterioration typically begins subtly in midlife, it can accelerate over time through compounding cycles of disuse, injury, or illness. Once this downward momentum gains speed, recovery becomes more difficult [58]. The same applies to cellular senescence: research shows that resistance training can delay the accumulation of senescent cells, reduce systemic inflammation, and enhance mitochondrial function—key mechanisms that help preserve cellular integrity as we age.
Those who engage in regular resistance training not only delay the onset of age-related disease but also maintain higher levels of independence and quality of life. By intentionally building reserves—both muscular and cellular—you extend your healthspan, not just your lifespan.
Backcasting is a powerful way to leverage research and known declines in physical capacity, strength, and/or power to estimate your own personal trajectory into the future. Based on some relatively quick math, you can establish present-day training targets to help guide your resistance exercise programming.
You love gardening, and you want to be able to confidently lift, move, and carry bags of landscaping materials, dirt, stone, or mulch as you surpass your 8th or 9th decade.
Backcasting Target: Considering each bag weighs approximately 40 to 50 lbs, you would need to set your sights on lifting that mass from the floor to approximately waist height.
Resistance Exercise Application: Next, consider the movement and match it with a similar resistance exercise movement, like deadlift or sandbag deadlift.
Performance Trajectory: To achieve the desired outcome, you now need to consider inevitable declines and build toward a present-day target that will allow you to maintain your ability into your 80s, 90s, and beyond. In this example, if your goal is to lift a 50 lb bag from the floor at 90 years, considering average declines in strength, you would need to be able to minimally be able to complete a 185.9 lb deadlift at age 30. Factoring in some headspace as a buffer for unexpected injuries, illness, or gaps in regular training, a comfortable target that is 25% greater would be a 232.4 lb deadlift at 30 years old. If you can push your peak past this, you improve your likelihood of surpassing your Backcasting Target over the next 5-6 decades.
Backcasting is a beneficial strategy to guide resistance exercise training for most individuals who do not focus on competitive exercise or sport performance in the present. Rather than reactive avoidance, backcasting can give you a clear direction to proactively pursue goals that fit with inevitable declines in muscle health and function based on valuable research data in humans. Establishing benchmarks that are linked with long-term goals is a powerful way to personalize your resistance training program as you train to improve muscle health, protect yourself from excessive cellular senescence, and enjoy the benefits of your investment in longevity.
TAKE HOME POINTS
Aging processes linked to cellular senescence can be influenced through lifestyle, pharmacological, and environmental interventions.
Although senescent cells are initially protective, they contribute to declines in healthy tissue and organ function when they accumulate over time.
Lifestyle interventions (exercise and nutrition) in humans can effectively attenuate comorbidities and cellular senescence/immunosenescence that accelerate aging linked with autoimmune conditions.
Consistent habitual resistance and endurance exercise training has been shown to mitigate cell senescence throughout the body, not only in active skeletal muscle.
Skeletal muscle is a pivotal, arguably one of the most important longevity organs.
Active muscle releases myokines that can have stimulatory and inhibitory effects. There are over 3000 myokines, and research continues to uncover unique mechanisms whereby they target aging and senescence.
Resistance exercise training 3 days per week for 5 months has been shown to reduce senescent cell abundance in thigh adipose tissue by 60% in female participants with an average age of 72 years.
Acute resistance exercise produces significant leukocyte infiltration in muscle as well as a 50% reduction in p16(INK4a) positive senescent cells.
Age-related declines in muscle mass, strength, and power are inevitable, however, resistance training can improve trajectory and ultimately may prevent falling below clinical thresholds for sarcopenia, osteoporosis, and frailty.
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.