The Role of Rapamycin (Sirolimus) in Treating and Normalizing Cell Growth in Keratosis Pilaris
Understanding KP: Keratosis Pilaris (KP) is a common skin condition characterized by dry, rough, and bumpy skin, often due to the accumulation of keratin in hair follicles.
Current Treatments: Traditional management options for KP include emollients, keratolytics, corticosteroids, and retinoids, which primarily focus on alleviating symptoms but do not address the root cause.
mTOR's Importance: mTOR (mechanistic Target of Rapamycin) regulates cell growth and metabolism. Hyperactivity of mTOR is linked to various conditions, including KP.
Rapamycin's Potential: mTOR inhibitors like rapamycin can target the underlying cause of KP by reducing mTOR activity, normalizing cell growth, and decreasing excessive keratin production.
Case Study Evidence: A study on a 15-year-old patient demonstrated significant improvement in KP symptoms using 1% topical rapamycin cream, indicating its effectiveness and safety as a treatment option.
Future Research: Further exploration into mTOR inhibitors could transform the management of KP and similar conditions, highlighting the need to address root causes for more effective and lasting results.
Keratosis Pilaris (KP), commonly known as "chicken skin," manifests as dry, rough, and bumpy patches on the skin, often causing significant discomfort and cosmetic concern. Traditional treatments primarily manage symptoms without addressing the root cause, leaving many patients seeking more effective solutions.
Recent advancements in dermatological research have introduced a novel application of rapamycin, an mTOR inhibitor, in treating KP. By targeting the mTOR pathway, rapamycin helps normalize cell growth and reduce keratin buildup, which is central to KP's pathology.
This article delves into this innovative approach, presenting a case study where a 15-year-old patient achieved significant and sustained improvement in skin texture and redness after applying a 1% topical rapamycin cream over 18 months. This promising treatment highlights rapamycin's potential to offer a more effective and lasting solution for KP, shifting the focus from symptom management to addressing underlying cellular mechanisms. This exploration not only opens new avenues for KP treatment but also enhances our understanding of mTOR's role in skin health, suggesting broader implications for dermatological therapies.
What is Keratosis Pilaris (KP)?
Keratosis Pilaris (KP), commonly known as "chicken skin," is a benign skin condition characterized by dry, rough, and bumpy skin. It can occur at any age but is most prevalent in young children. The primary symptoms include small, painless bumps on the upper arms, thighs, cheeks, or buttocks. These bumps, which may be skin-colored, white, or red, can sometimes be itchy or feel dry. KP tends to worsen during seasons with low humidity, contributing to drier skin conditions. The exact etiology of KP remains unclear, but it is thought to result from a combination of genetic predispositions and environmental factors such as changes in temperature and humidity. Individuals with dry or sensitive skin are particularly susceptible to developing this condition. [1]
While Keratosis Pilaris (KP) is often more prominent in children, it can persist into adulthood for many individuals. In some cases, the symptoms of KP may diminish with age, but adults can continue to experience the characteristic rough, bumpy texture of their skin. For adults, KP often remains a chronic condition with varying degrees of severity that may fluctuate with seasonal changes and skin care routines. Although the condition does not have a cure, several practices can help alleviate its symptoms and improve the skin's appearance. [1]
Underlying Mechanisms of KP
The bumps associated with Keratosis Pilaris (KP) are sometimes mistaken for small pimples; however, they differ significantly from acne. These bumps develop due to an accumulation of keratin, a protein responsible for skin exfoliation. When keratin builds up, it clogs the hair follicles—small, tube-like structures in the skin that produce hair. This accumulation traps hair strands within the follicles, leading to the rough, bumpy texture characteristic of KP. [2]
Although the exact cause of KP remains unclear, it frequently co-occurs with other dry skin conditions, enhancing its visibility and symptoms. One such condition is Ichthyosis Vulgaris (IV), a genetic disorder where the body produces a defective version of the protein filaggrin, which is crucial for skin cell shedding. This defect makes it difficult for individuals with IV to shed dead skin cells, resulting in dry, scaly, and thickened skin. Another related condition is xerosis, known as dry skin, which can affect individuals of any age and skin type.
Environmental factors such as low humidity, cold weather, harsh soaps, and excessive bathing can exacerbate this condition. Similarly, atopic dermatitis (AD), also known as eczema, contributes to the challenges associated with dry skin. AD is a chronic inflammatory condition characterized by intensely itchy rashes that recur and often appear on various body parts, including the face, hands, elbows, and knees. These rashes lead to dry, scaly skin, further complicating the management of KP. [2]
Current Management Strategies Options for KP
Managing Keratosis Pilaris (KP) involves a combination of skincare and medication tailored to alleviate symptoms rather than cure the condition. Gentle, moisturizing skincare products, avoiding harsh scrubbing, and maintaining well-hydrated skin are foundational practices. Additionally, the treatments listed below can significantly help manage symptoms; however, their effectiveness varies, and they are not curative. [3]
- Emollients: Emollients are crucial in creams, lotions, moisturizers, or ointments that create a protective barrier on the skin's surface. This barrier soothes dryness, itching, and flaking and helps retain moisture, which is essential for softening the skin and reducing the rough texture typical of KP. Products like CeraVe Moisturizing Cream, Eucerin Advanced Repair Cream, and Aveeno Daily Moisturizing Lotion can improve skin appearance and texture, though they do not cure KP. [3]
- Keratolytics: Keratolytics, such as salicylic acid (SA) and lactic acid (LA), facilitate the removal of dead skin cells by softening and dissolving the outer skin layer. These agents are beneficial for treating conditions marked by excessive keratinization, such as KP, acne, and psoriasis. Research, including a study by Kootiratrakarn et al. (2015), shows that treatments like 10% LA and 5% SA creams can significantly reduce KP lesions and are generally well-tolerated. Still, they are not a cure, and results may vary. [4]
- Corticosteroids: Corticosteroids have anti-inflammatory properties and alleviate inflammation and itching associated with KP, particularly when aggravated by scratching. While topical corticosteroids can temporarily relieve symptoms like redness and discomfort, they must be used cautiously under medical supervision due to risks such as skin thinning and pigmentation changes, and they do not provide a permanent solution. [3]
- Retinoids: Retinoids work by unclogging pores and promoting the turnover of skin cells, thus smoothing skin texture and reducing the visibility of bumps. Prescription retinoids like tretinoin (Retin-A), adapalene (Differin), and tazarotene (Tazorac), as well as over-the-counter retinol, can be effective. However, their potency varies and is not a definitive cure for KP. [3]
While these treatment options can manage the symptoms of Keratosis Pilaris and improve skin condition, they work to varying degrees, and none offer a cure. The goal is to enhance comfort and appearance, adapting treatment plans to individual needs and responses.
Laser-Therapy - The Current Research-Backed Solution
In addition to the options above, current Keratosis Pilaris (KP) treatments also involve laser therapy. One such treatment is quality-switched QSNd: YAG technology. The QSNd: YAG laser works by targeting and breaking down excess keratin, helping to reduce the appearance of the bumps. The energy from the laser is specifically absorbed by the excess keratin, allowing for selective removal without damaging the surrounding healthy skin. The laser can also help reduce any redness or inflammation associated with KP, further improving the appearance of the skin. [5]
Several studies have examined the efficacy of QSNd: YAG laser technology in managing KP. One such study, conducted by Park et al. in 2011, evaluated the clinical response of KP to this laser treatment, with a particular focus on assessing the effects on skin pigmentation and smoothness. [5]
The study involved 12 patients who received ten laser sessions over five months. The results were quite promising. Eleven out of the twelve patients, or 91.7%, saw at least a 25% improvement in their skin's texture and discoloration. Furthermore, about half of the patient cohort, six individuals, demonstrated over 50% improvement in skin texture. A similar proportion, 42% (five patients), exhibited more than 50% improved skin discoloration. Notably, the majority of participants, eleven out of twelve, expressed satisfaction with the treatment. No significant adverse effects were reported throughout the study. Overall, the study demonstrated that Q-switched Nd: YAG laser treatment is an effective modality for improving the appearance of KP, with high patient satisfaction and tolerability. [5]
In addition to QSNd: YAG technology, other laser technologies are also gaining recognition. Another popular state-of-the-art technology is the fractional CO2 laser. The laser creates microscopic columns of thermal injury called microthermal zones (MTZs) in the skin. These MTZs penetrate the deeper layers of the skin, targeting the keratin deposits that trigger the bumpy appearance in KP. The laser energy helps break down and remove excess keratin, promoting the exfoliation of dead skin cells. [5]
Apart from discharging keratin deposits, the treatment stimulates the skin's natural wound-healing response, increasing collagen production. Collagen is a natural protein our bodies produce that keeps the skin supple and youthful-looking by providing elasticity and firmness. By promoting collagen production, CO2 lasers help improve the skin texture of individuals with KP. [5]
Ismail et al. (2020) investigated the efficacy, safety, and tolerability of fractional CO2 lasers in managing KP. The study involved 60 patients with KP on their arms (group A) and thighs (group B). One side of their arms or thighs was randomly chosen for laser treatment, and the other side was treated with a topical keratolytic cream. The patients came in for two laser treatment sessions, with four weeks in between. The researchers took photos of the skin at each visit to evaluate the improvement.
Overall, the results showed that the laser treatment improved the KP on both the arms and thighs. For the arm group (A), ten patients (33.3%) had excellent improvement, eighteen patients (60%) had good improvement, and two patients (6.7%) had moderate improvement after the second treatment. For the thigh group (B), two patients (6.7%) had minimal improvement, sixteen patients (53.3%) had moderate improvement, and twelve patients (40%) had good improvement. The side of the skin that only received the topical cream showed only minimal improvement, mainly on the arm lesions. Notably, the patients were much more satisfied with the results on the laser treatment side than the side that only received the topical cream. [6]
A diode laser is a third type of laser currently used in the KP landscape. Diode lasers target concentrated energy to keratinized follicles and create microscopic wounds in the skin. This process helps to remove the top layer of dead skin cells and promotes the growth of new, healthier skin cells. The improved skin cell turnover helps reduce the appearance of the rough, bumpy texture associated with the condition. Like CO2 lasers, diode lasers also promote collagen production to improve further the texture and appearance of skin affected by KP. The efficacy of diode lasers in treating KP has been well-documented in several studies. One such study, conducted by Ibrahim et al. in 2015, explored using a diode laser. [7]
The study involved 18 patients with KP on both arms and light to medium skin tones. The researchers treated one arm of each patient with the laser, with sessions spaced 4-5 weeks apart, for three treatments. After 12 weeks, two dermatologists, unaware of which arm had received the laser treatment, evaluated the skin on each arm, assessing the redness and roughness/bumpiness on a scale of 0 (least severe) to 3 (most severe). The results showed that the laser treatment significantly improved the roughness and bumpiness of the skin, with a difference of 1 point on the severity scale between the treated and untreated arms. [7]
Laser therapies have emerged as a promising treatment option for managing Keratosis Pilaris (KP). However, they do not come without side effects. Potential side effects of laser treatments for KP can include temporary redness, swelling, and discomfort in the treated area. Some patients may experience hyperpigmentation or hypopigmentation, where the skin becomes darker or lighter, particularly in individuals with darker skin tones. There's also a risk of blistering, scarring, or infection if the post-treatment care is not adequately followed.
With this side effect profile, there is a need for alternative therapies to manage Keratosis Pilaris (KP) effectively. [5]
Gaps in Current Treatment Choices for KP
As Keratosis Pilaris (KP) management continues to evolve, further research is needed to fully explore the potential of topical supplements and innovative laser technologies in relieving individuals with this common skin condition. [9]
Although treatment options continue to expand, some gaps and limitations remain. One primary issue is the variability in response to treatment. A treatment that works wonders for one person may not necessarily be effective for another, making it challenging to find the optimal choice for each individual. Another gap is the lack of long-term durability. While effective in the short term, many current treatment options may not provide long-lasting results. KP's bumps and rough texture often reappear after treatment is stopped or discontinued. Indeed, many patients who undergo laser therapies, including QS Nd: YAG, diode, and CO2 lasers, commonly report experiencing adverse side effects, such as dysregulated coloration, redness, and swelling of the skin. [5] [6]
Besides long-term durability, there is also a lack of preventative focus. Current options mainly manage the visible symptoms of KP, but there are no effective strategies to prevent the recurrence of the condition. The cost of current treatment choices is another major limitation. Specialized treatment options, such as advanced laser therapies, may not be readily available or accessible to all patients, especially those in underserved or resource-limited areas.
Finally, in many cases, a single treatment modality may not address the various aspects of KP. For example, in the study by Ibrahim et al. (2014), the diode laser helped reduce the bumpy, rough appearance of the skin in the patient cohort. However, it did not improve redness and/or inflammation. This highlights the need for comprehensive treatment approaches that effectively address all symptoms of KP.
Mammalian Target of Rapamycin (mTOR) Inhibitors - A Novel Approach
As discussed in our previous articles, mTOR (mechanistic Target of Rapamycin) is often called the master regulator of cell growth and metabolism. This protein kinase is critical in integrating signals from nutrients, growth factors, and cellular energy levels to control cell proliferation, growth, and survival. By coordinating these signals, mTOR ensures that cells grow and divide only when optimal, thus maintaining cellular and tissue homeostasis. [8]
Current treatments for keratosis pilaris (KP) often focus merely on alleviating symptoms rather than addressing the condition's underlying cause. There is a significant gap in treatment strategies that fail to target a root cause of KP—namely, the hyperactivity of mTOR. When mTOR becomes hyperactive, it can lead to various cellular dysfunctions. Excessive nutrient intake, chronic inflammation, genetic mutations, and the natural aging process can trigger this hyperactivity. When mTOR is overly active, it can drive unchecked cell growth and proliferation, which is linked to skin conditions like KP. [2]
To address conditions like KP and other health issues associated with mTOR hyperactivity, mTOR inhibitors, such as Rapamycin, can be a vital tool. Rapamycin works by inhibiting the mTOR pathway, thereby reducing the activity of mTOR. This inhibition helps to normalize cell growth and proliferation. In the context of KP, Rapamycin can reduce the excessive keratin production in the skin. This can help alleviate the rough bumps by promoting healthier skin cell turnover and reducing the buildup of keratin. [9]
In one specific case study, researchers tested the effectiveness of a 1% topical rapamycin treatment on a 15-year-old patient. The patient had persistent and worsening redness, small bumps on his cheeks, neck, and arms, and a burning sensation. His condition worsened following exposure to wind and flushing. Previously, he had been diagnosed with KP and was given ammonium lactate 12% lotion and tretinoin (retinoid) 0.1% microsphere gel, but these treatments provided no improvements. Common treatments, including emollients, keratolytics, lactic acid, salicylic acid, retinoids, corticosteroids, and vitamin-D analogs, are often ineffective for many patients with this form of KP. [9] [10][11]
The patient in this study was asked to apply a 1% topical rapamycin cream twice daily to the affected areas for two months, followed by a daily application for 14 months. Eighteen months later, the redness and bumps on his face and neck were completely resolved (see Figures 1 and 2). When asked about the treatment, the patient mentioned that he observed significant improvements after two months of applying the cream twice daily. He managed to sustain these results by applying the cream only once daily for several months. To investigate the safety of the treatment, the patient's serum sirolimus levels were also obtained, revealing a less than three ng/mL sirolimus amount, which is clinically insignificant. Hence, the study marked sirolimus 1% topical cream as a safe and effective treatment strategy for KPR. [10][12]
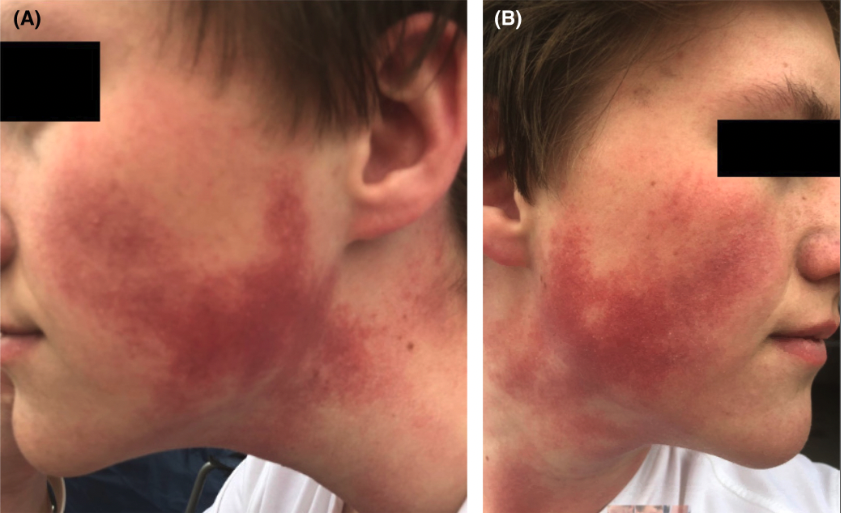
Figure 1 (A, B): Skin and neck redness and texture before topical 1% Sirolimus cream. The patient's cheeks and neck show small, uniform bumps that have coalesced into large, reddish-purple areas with increased blood flow. This appearance is typical of KP Rubra. [9]
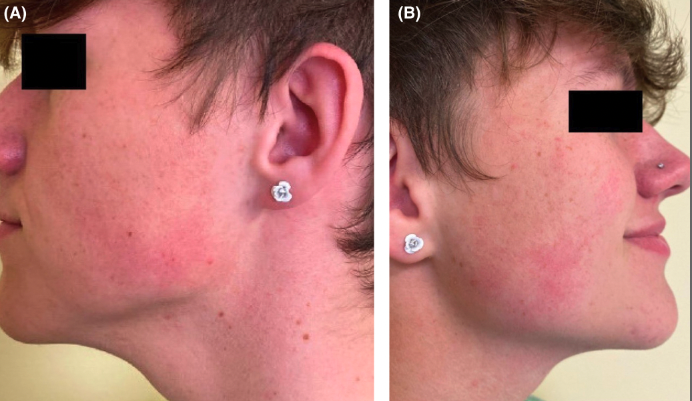
Figure 2 (A, B): Skin and neck redness and texture following 14-month topical 1% Sirolimus cream application. Facial redness and painful burning sensations resolved. [9]
Conclusion
While traditional keratosis pilaris (KP) treatments have focused on managing symptoms, addressing the root cause offers a promising new direction. The effectiveness of mTOR inhibitors like Rapamycin highlights the potential of targeting the underlying mechanisms of KP rather than merely alleviating its symptoms. This novel approach provides significant and sustained improvement and opens up new avenues for understanding and treating other conditions linked to mTOR hyperactivity. Continued research into mTOR inhibition could change the management of KP and similar dermatological issues, emphasizing the importance of tackling the root causes of such conditions for more effective and long-lasting results.
- Clinic, M. (2024, February 17). Keratosis pilaris. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/keratosis-pilaris/symptoms-causes/syc-20351149#:~:text=Keratosis%20pilaris%20(ker%2Duh%2D,t%20be%20cured%20or%20prevented.
- Hwang, S., & Schwartz, R. A. (2008). Keratosis pilaris: a common follicular hyperkeratosis. Cutis, 82(3), 177–180.
- Marqueling AL, Gilliam AE, Prendiville J, et al. Keratosis pilaris rubra: a common but underrecognized condition. Arch Dermatol. 2006;142(12):1611- 1616
- Kootiratrakarn, T., Kampirapap, K., & Chunhasewee, C. (2015). Epidermal permeability barrier in the treatment of keratosis pilaris. Dermatology research and practice, 2015, 205012.
- Park, J., Kim, B. J., Kim, M. N., & Lee, C. K. (2011). A Pilot Study of Q-switched 1064-nm Nd: YAG Laser Treatment in the Keratosis Pilaris. Annals of Dermatology, 23(3), 293–298. https://doi.org/10.5021/ad.2011.23.3.293
- Ismail, S., & Omar, S. S. (2020). Clinical and dermoscopic evaluation of fractional carbon dioxide laser in the management of keratosis pilaris in Egyptian type skin. Journal of cosmetic dermatology, 19(5), 1110–1120. https://doi.org/10.1111/jocd.13140
- Ibrahim, O., Khan, M., Bolotin, D., Dubina, M., Nodzenski, M., Disphanurat, W., Kakar, R., Yoo, S., Whiting, D., West, D. P., Poon, E., Veledar, E., & Alam, M. (2015). Treatment of keratosis pilaris with 810-nm diode laser: a randomized clinical trial. JAMA dermatology, 151(2), 187–191. https://doi.org/10.1001/jamadermatol.2014.2211
- Bakhshi, S. (2023, October 22). Healthspan Research Review: Rapamycin Research and clinical trials: A synthesis of recent scientific findings. Healthspan. https://gethealthspan.com/science/article/rapamycin-research-synthesis-recent-scientific-findings
- Eckburg, A., Kazemi, T., & Maguiness, S. (2022). Keratosis pilaris rubra successfully treated with topical sirolimus: Report of a case and review of the literature. Pediatric dermatology, 39(3), 429–431. https://doi.org/10.1111/pde.14963
- Marqueling AL, Gilliam AE, Prendiville J, et al. Keratosis pilaris rubra: a common but underrecognized condition. Arch Dermatol. 2006; 142(12): 1611-1616.
- Schoch JJ, Tollefson MM, Witman P, Davis DM. Successful treatment of keratosis pilaris rubra with pulsed dye laser. Pediatr Dermatol. 2016; 33(4): 443-446.
- Dodds M, Tollefson M, Castelo-Soccio L, et al. Treatment of superficial vascular anomalies with topical sirolimus: a multicenter case series. Pediatr Dermatol. 2020; 37(2): 272-277.
Related studies