.png?u=https%3A%2F%2Fimages.ctfassets.net%2Fzvzqa1d1gh0f%2F68YrPbjn5g7t8jFrx2OLuQ%2Fb206487615608c4585c6e309d8dd9567%2Flabs_2__1_.png&a=w%3D55%26h%3D55%26fm%3Dpng%26q%3D75&cd=2025-06-12T20%3A31%3A13.529Z)
Heart Vitality Panel
The Heart Vitality Panel goes beyond traditional lipid tests, it provides a comprehensive view of heart health risks, empowering proactive care with precision.
Belly fat has earned a notorious reputation associated with looming health risks. But when we look closer, we discover a surprising twist: not all belly fat is the enemy. Specifically, the soft, pinchable layer just below the skin—known as abdominal subcutaneous adipose tissue (abSAT)—can actually play a protective role. Picture abSAT as your body’s energetic “savings account”: when you’re not eating, it breaks down stored fat to power the body; when you do eat, insulin steps in to curtail that breakdown and encourage new fat storage. This constant give-and-take is part of a finely tuned system that keeps metabolism running smoothly—until obesity complicates the picture. For many, the inability of abSAT to properly store fat leads to a detrimental spillover of lipids into other tissues, contributing to insulin resistance and chronic disease. Yet here’s the paradox: some people with obesity remain remarkably healthy, suggesting that their abSAT expands without jeopardizing insulin signaling or metabolic balance. In this review, we follow the thread of new research unveiling how regular endurance exercise helps abSAT stay flexible in individuals with obesity. We’ll explore how increased capillary density, reduced fibrosis, and a more favorable immune cell environment allow abSAT to function as a stable reservoir for fat—even under the strain of extra weight. Finally, we’ll introduce specific endurance exercise strategies shown to nurture this healthy fat storage capacity across the lifespan, reframing our understanding of belly fat from a universal villain to a potential metabolic ally.
Exercise
Anti-Inflammation
health
science
longevity
21 mins
By: Dr. Aaron L. Slusher
Fat, or adipose tissue, is among the most misunderstood organ systems within the body. Although it is often discussed as a single entity, multiple distinct forms of adipose tissue exist with unique functions. Of its several types, subcutaneous adipose tissue (SAT) is the pinchable fat distributed across the body and found underneath the skin. The distribution of SAT is not evenly spread across the body, and a few locations, such as the breasts, buttocks, and abdomen, are associated with the increased storage relative to other sites, including the cheeks and lower arms. For decades, SAT was considered a passive location for excess fat storage and has been the subject of many medical and cultural misconceptions regarding health.
Recent research has begun to bring many of these misconceptions to light, indicating that what we once believed about SAT is not entirely accurate. In fact, a 2024 study in Nature Metabolism shed light on the plasticity of abdominal fat storage [1], demonstrating that abdominal fat is a keystone organ that helps maintain overall metabolism and healthy aging.
It is now well understood that SAT regulates the secretion of appetite-regulating hormones, provides insulation to maintain body temperature, and serves as a layer of protective cushioning for the body. Increasingly more evidence also supports SAT as a healthy location for fat storage, and its ability to balance fat breakdown (lipolysis) and storage (lipogenesis) highlights a novel mechanism to maintaining metabolic health in response to decreased or increased nutrient availability, respectively.
Building on these insights, lifestyle strategies that optimize SAT’s beneficial role have drawn increasing interest, with endurance exercise emerging as a particularly effective approach. Jeffrey Horowitz's laboratory at the University of Michigan School of Kinesiology has long examined the mechanisms that underpin this relationship. Their most recent study, entitled “Years of Endurance Exercise Training Remodel Abdominal Subcutaneous Adipose Tissue in Adults with Overweight or Obesity,” details two critical findings among two populations with obesity. First, the structure of SAT stored in the belly region, termed abdominal (ab)SAT, differs among individuals who regularly participate in endurance exercise compared to those who are sedentary. Second, these changes alter the function of abSAT and help explain how endurance exercisers remain metabolically healthy compared to sedentary individuals with varying levels of insulin resistance.
In this review, we will detail the findings from this investigation, helping to reshape our thinking around fat storage and changing the narrative surrounding the presence of belly fat as a cultural indicator of health. Additionally, we will provide a practical overview of how endurance exercise can be utilized as a behavioral strategy to improve fat health in all individuals, regardless of current weight, aiming to maintain their metabolism throughout aging.
In the fasted state, hormones such as growth hormone, cortisol, and catecholamines stimulate the breakdown of fats stored as triglycerides into their primary components: a glycerol molecule and three fatty acids. Both glycerol and the three newly formed fatty acids enter circulation, where they help the liver produce glucose through a process called gluconeogenesis [2]. This newly produced glucose serves to maintain plasma concentrations and provide the body with fuel for energy metabolism. In addition, the fatty acids travel to various organs to be metabolized and utilized as fuel inside a cell’s mitochondria.
Fat storage is vital to maintaining energy availability in a fasted state. Current estimates suggest that about 90% of circulating fatty acids are secreted by the SAT, and nearly 70% derive from abdominal SAT [3].
Abdominal SAT has been referred to as “exquisitely sensitive” to the hormone insulin [2]. Food consumption that increases blood glucose concentrations stimulates insulin release by the pancreas. Upon insulin binding to its receptor on the fat cell (adipocyte) surface, the breakdown of stored fats is rapidly inhibited, the release of fatty acids into circulation is decreased, and fat storage is increased. In fact, post-meal insulin concentrations inhibit fat breakdown by about 90% within 5-10 minutes under healthy metabolic states [2, 4]. However, when fat cells are resistant to insulin, the breakdown of fat continues for longer and sequelae of metabolic disease can accelerate.
Obesity is a condition associated with the inability of insulin to inhibit the breakdown of fat. In the presence of fat cell insulin resistance, excess fatty acids enter circulation and are stored in areas that surround internal organs (referred to as the visceral adipose tissue) as well as within other tissue types, such as the liver, heart, and skeletal muscle. Excess fat accumulation in these locations can cause whole-body insulin resistance and accelerate age-related disease progression, such as type 2 diabetes, cardiovascular disease, Alzheimer’s disease, and various types of cancers [5-8].
Most individuals with obesity exhibit insulin-resistant abdominal subcutaneous adipose tissue (abSAT). However, a conservative estimate indicates that ~10-30% of individuals with obesity remain insulin sensitive, metabolically healthy, and do not experience the same degree of disease pathology as their insulin-resistant counterparts [9, 10]. A potential explanation is that metabolically healthy individuals with obesity have abSAT that retain their ability to expand and increasingly store fat when necessary. Increasing abSAT storage capacity is the product of two processes:
Adipogenesis – New fat cell formation occurs when immature fat cells (preadipocytes) turn into new, mature fat cells. This process helps increase the total number of fat cells available to store fat within a specific location.
Hypertrophy – Increasing the size of an individual fat cell through expansion allows for more total fat to be stored within each cell.
The current view is that expanding the size of individual fat cells is key to abSAT functioning as a metabolically healthy location for fat accumulation [11]. By safely housing excess fat within abSAT during periods of nutrient excess, the body can avoid depositing it in or around other vital organs where it can drive harmful metabolic effects and is associated with increased risk for type 2 diabetes, cardiovascular disease, and premature death [10, 11]. In fact, preserving the sensitivity of abSAT to insulin has been shown to maintain the balance between fat breakdown and storage, even in the presence of excess fat storage and weight gain [12]. Therefore, understanding these mechanisms is extremely important to preventing the progression from metabolically healthy to unhealthy, which occurs in ~30-50% of individuals with obesity over a 4-20 year period [13].
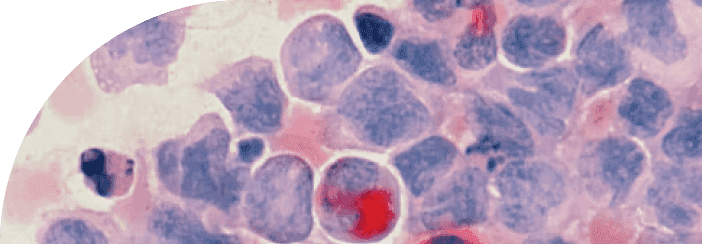
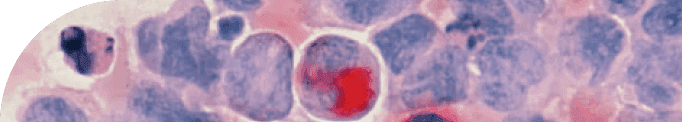
Specific physical and morphological characteristics of abdominal subcutaneous adipose tissue (abSAT) and the surrounding microenvironment may underlie adipose tissue expansion capacity, insulin sensitivity, and predict whether an individual maintains a healthy metabolic profile [14]. As a result, three areas of research have gained the most attention:
Capillary density – The number of blood vessels that are near and surround the individual fat cell (adipocyte). Increased capillary density, a product of angiogenesis, stems from forming new blood vessels and helps increase blood flow to individual adipocytes. Greater blood flow can help deliver oxygen and nutrients while removing waste products more efficiently.
Extracellular matrix remodeling – Collagen forms a scaffolding around an individual or group of fat cells and provides a structural framework to support increased abSAT mass. Excessive fibrous, collagen-like proteins can restrict the ability of fat cells to expand and store lipids.
Resident macrophage – Immune cells that reside within abSAT and help determine the presence of a pro-inflammatory or anti-inflammatory microenvironment. Their inflammatory profile can impact the concentration of pro- and anti-inflammatory proteins secreted into circulation.
Not surprisingly, endurance exercise training has emerged as one of the most impactful behavioral strategies to positively alter abSAT and improve overall metabolic health among healthy individuals [15]. More recent research published in 2022 suggests that as few as 12 weeks of moderate and high-intensity endurance exercise training is sufficient to elicit positive structural and functional adaptations to abSAT among individuals with obesity, even in the absence of weight loss [16].
New research from Dr. Jeff Horowitz’s laboratory at the University of Michigan published in Nature Metabolism expands our understanding of endurance exercise as a behavioral strategy to improve abdominal subcutaneous adipose tissue (abSAT) function and maintain metabolic health in the presence of obesity. This study demonstrates that individuals with obesity who engaged in two years of regular endurance exercise training have increased capillary density, decreased extracellular matrix fibrosis, and more favorable macrophage profiles compared to their sedentary counterparts with obesity [1]. In addition, the improved abSAT structure paralleled more advantageous fat storage capacity and insulin sensitivity among endurance exercisers with obesity.
In this study, 52 individuals with overweight or obesity were selected. Subjects were split into two groups: 28 subjects were classified as sedentary or physically inactive, and 24 self-reported as endurance exercisers (at least 4 days per week for two or more years). To control for the potential impact relating to differences in body composition, a final sample of 16 individuals (8 females and eight males) were selected for each study group and matched for age, body weight, body mass index (BMI), and body fat percentage and mass. As expected, absolute and relative VO2 peaks, two indices of cardiorespiratory fitness, were greater in the endurance exercise group.
Following an overnight fast, blood samples were obtained upon arrival, and a small amount of abSAT was biopsied and flash-frozen to preserve tissue integrity. Collected abSAT samples were utilized to examine potential differences in the presence and density of blood capillaries, extracellular matrix fibrosis, and indices of pro- and anti-inflammatory resident macrophages. Because no difference in body composition was present, researchers could identify the potential impact of habitual endurance exercise on abSAT structure, independent of differences in obesity and adiposity.
To uncover the specific ways endurance exercise enhances abSAT health, the authors focused on three main structural features: capillary density, extracellular matrix remodeling, and resident macrophages.
Capillary Density
Capillary density and protein expression of vascular endothelial growth factor α, a master regulator of new blood vessel formation [17], were significantly higher among endurance exercisers compared to sedentary individuals. This increased vascular network functions similarly to the local roadways that help you travel to a wider area within a community and make services like the delivery of goods or the removal of waste more efficient. And just as these roadways help support connectivity of growing communities, increased vascular networks within fat cells is necessary to support their expansion. Therefore, these results suggest that endurance exercise elicits the continual formation of new vascular networks to ensure sufficient delivery of nutrient-rich, oxygenated blood throughout the abSAT, while also enhancing the removal of metabolic by-products at rest and during physical activities.
Extracellular Matrix Remodeling
The extracellular matrix (ECM) is the supportive framework that surrounds fat cells. Think of it like scaffolding: in healthy tissue, this scaffolding is flexible, allowing fat cells to expand and contract as needed. But in obesity, the ECM often becomes stiff and overbuilt—particularly due to the accumulation of collagen proteins like collagen type XVI alpha 1 (Col16a1). When this happens, fat cells lose their ability to grow properly, which can lead to inflammation, poor blood flow, and insulin resistance.
In this study, individuals who regularly performed endurance exercise had significantly lower levels of Col16a1 in their abdominal fat tissue compared to sedentary individuals [18]. This suggests that regular aerobic exercise helps break down excess collagen and prevents the development of a fibrotic, unhealthy fat environment.
Interestingly, the study also observed a trend toward higher levels of matrix metalloproteinase-14 (MMP14) among endurance exercisers. Although this difference was not statistically significant, MMP14 is known to break down Col16a1, suggesting that endurance exercise may activate a remodeling process in which fibrotic proteins are cleared away. This remodeling makes the ECM more flexible and allows fat cells to expand in a healthier way when extra energy storage is needed.
Why does this matter? In a fibrotic fat environment, when fat cells can’t expand, excess lipids are redirected to other organs like the liver, heart, and muscle—where they contribute to metabolic disease. By contrast, a more adaptable ECM allows fat tissue to function properly as a safe storage depot, reducing systemic metabolic strain.
Macrophage Profiles and Immune Modulation
The study found that endurance exercisers had lower levels of both CD14-expressing pro-inflammatory macrophages and CD206-expressing anti-inflammatory macrophages within their abdominal subcutaneous fat (abSAT) [1]. This pattern contrasts with previous rodent studies, which have often shown that exercise causes a shift from pro-inflammatory to anti-inflammatory macrophages in adipose tissue [19, 20]. Instead of supporting that polarization model, the findings from this study suggest that endurance exercise in humans may lead to a more generalized reduction in immune cell infiltration into fat tissue.
The authors propose that this broad decrease in macrophages might reflect an overall reduction in local immune activation within the fat depot. In line with this idea, they also observed lower expression of genes involved in the complement system—an early-acting arm of the innate immune response that plays a key role in recruiting immune cells like macrophages to tissues [1]. By dialing down complement activity, endurance exercise may reduce immune cell recruitment into fat tissue, which could help dampen chronic, low-grade inflammation commonly seen in obesity.
Interestingly, while these local changes in immune cell populations were clear within abSAT, there were no significant differences in circulating inflammatory cytokines between the two groups. This suggests that endurance exercise may exert its anti-inflammatory effects in a tissue-specific manner—improving the immune environment of fat tissue without necessarily altering systemic inflammatory markers .
Together, these findings suggest that endurance exercise may improve fat tissue health not by selectively increasing anti-inflammatory macrophages, but by reducing the overall immune burden within the tissue [21]. This more “quiet” immune environment may help protect against the chronic inflammation and metabolic dysfunction associated with obesity [1].
Each of the adaptations described above—enhanced capillary density, reduced ECM fibrosis, and decreased immune cell infiltration—represent metabolically favorable changes to both adipocytes and their surrounding environment within abdominal subcutaneous adipose tissue (abSAT). However, a key question remains: do these structural improvements actually enhance the functional capacity of fat tissue—specifically, its expandability (the ability of adipocytes to grow without dysfunction) and storage capacity (the ability of abSAT to safely sequester excess energy as lipid)? These properties are essential because when fat tissue loses its ability to expand or store lipids effectively, excess fat is redirected into organs like the liver, heart, and muscle, driving insulin resistance and metabolic disease. Demonstrating improved expandability and storage in this context would provide critical evidence that endurance exercise not only remodels fat tissue structurally but also restores its ability to act as a metabolically protective buffer against lipid overflow and systemic dysfunction.
Likewise, the downstream implications of these structural and functional changes on overall metabolic health remain unknown. In the same study, Ahn and researchers performed a second experiment aiming to address these lingering questions [1].
A larger sample of age, sex, and BMI-matched sedentary (n = 24) individuals presenting with elevated body fat percentage and total fat mass were compared to the endurance exercise group (n = 19) [1]. Although subsequent analysis was controlled for the level of obesity as determined by BMI, body composition differences may have impacted the interpretation of the results. Nonetheless, two key experiments were carried out on fresh abSAT samples to examine how fat cells build new capillary networks and store fat. By examining these functions in an artificial environment, researchers can gain necessary insight into how these cells may function within the body under similar conditions.
Fresh abSAT samples from both groups were cultured in the presence of specialized growth media designed to stimulate either the development of new vascular networks (angiogenic activity) or determine the storage capacity of fat cells [1].
After 11 days, abSAT samples from endurance exercisers displayed a greater number of new vascular “sprouts” compared to sedentary individuals. Likewise, abSAT expansion and fat storage capacity was also greater among endurance exercisers compared to sedentary counterparts after nearly 4 weeks. These findings provide functional confirmation that structural remodeling in response to endurance exercise directly enhances the ability of fat tissue to expand and store lipids safely—an essential mechanism for protecting against ectopic fat accumulation and metabolic disease.
Interestingly, gene expression analysis of the cultured abSAT samples provided molecular evidence supporting these structural and functional improvements [1]. Compared to sedentary individuals, endurance exercisers showed higher expression of genes involved in triglyceride synthesis (DGAT1) and fat storage (SREBF1)—indicating that their fat tissue was more primed to safely store excess energy. At the same time, they had lower expression of genes associated with fibrosis (COL1A) and local inflammation (TNFα), suggesting a healthier, more metabolically supportive fat environment.
The researchers also assessed how participants responded to a standard oral glucose tolerance test—a measure of how efficiently the body handles a sugar load. Each research participant consumed a sugary beverage containing 75 grams of glucose, and blood samples were obtained every 15 minutes for two hours. Although glucose kinetics were similar between subject populations, the endurance exercisers required significantly lower concentrations of insulin released from the pancreas to regulate glucose in the blood and displayed reduced fatty acid concentrations in their blood compared to sedentary individuals.
Together, these findings reveal that endurance exercise not only improves the architecture of fat tissue—it also reprograms it at the molecular level to better store energy, regulate inflammation, and respond to hormonal signals like insulin. This combination may be critical for maintaining metabolic health in the presence of obesity.
Discussed together, each of the three primary endurance exercise-induced outcomes – increased capillary density, decreased extracellular matrix fibrosis, and decreased local inflammatory profiles – all positively modify the microenvironment within abdominal subcutaneous adipose tissue (abSAT) fat to allow for the healthier storage of fat. More importantly, each adaptation points to the increased insulin sensitivity observed among endurance exercisers when compared to sedentary individuals.
Previous work by Ahn and colleagues showed similar adaptations to abSAT among otherwise sedentary adults with obesity following two separate exercise protocols lasting 12 weeks [16]. The first consisted of moderate-intensity endurance exercise performed continuously for 45 minutes at about 70% of maximal heart rate. The other protocol began with a 3-minute warm-up at 65% maximal heart rate, followed by 10 bouts of high-intensity interval exercise lasting 1 minute at 90% of maximal heart rate, separated by 1 minute of active recovery at a low intensity. After completion of the final interval, a 3-minute at 65% maximal heart rate was performed to end the session. Participants in both endurance exercise programs were allowed to select among cycling, treadmill running, elliptical machines, or rowing ergometers.
Both the moderate-intensity continuous and high-intensity interval exercise programs similarly improved body composition (decreased body fat percentage) and cardiorespiratory fitness (VO2peak) [16]. Likewise, both endurance exercise training protocols similarly increased capillary density, altered extracellular matrix profiles, and decreased average fat cell size. It is possible to suggest that high-intensity interval exercise may be a more time-efficient option, since these responses were elicited after just 25 total minutes of total exercise per session as opposed to 45 minutes required in the moderate-intensity, continuous exercise program. However, consistent participation, regardless of exercise type, frequency, and intensity, may be the most important factor in eliciting adaptations in abSAT in sedentary or physically inactive individuals.
As a general guideline, selecting a variety of exercises that you enjoy, at intensities equal to or greater than 70% maximal heart rate, and repeating them 3-4 times per week for 30-45 minutes per session consistently over time appears to be an effective endurance exercise strategy for improving and maintaining fat cell health. These recommendations also align with guidelines established by the American College of Sports Medicine and the Centers for Disease Control and Prevention: 90 minutes of high-intensity exercise or 150 minutes of moderate-intensity exercise per week.
Future Directions and Research Opportunities
A few key measures are missing from the current research analysis. First, differences in insulin resistance between endurance exercisers and sedentary individuals with obesity may stem from various factors relating to the insulin receptor itself. For example, the total number of insulin receptors at the fat cell surface may be decreased, lowering overall insulin sensitivity among sedentary individuals. In addition, the accumulation of diacylglycerols, glycerol molecules with two, as opposed to three fatty acids, at the plasma membrane of the fat cell impairs the activation of the insulin receptor and renders it less sensitive to insulin-mediated signaling [22]. Including these and other measures may highlight additional mechanisms to explain how endurance exercise maintains insulin sensitivity compared to sedentary, insulin-resistant individuals with obesity.
Secondly, only one measure of abdominal subcutaneous adipose tissue (abSAT) was obtained under resting conditions. Researchers highlight changes to proteins involved in fat breakdown (Akt and CGI-58) that were more apparent in exercisers compared to sedentary individuals. Previous research by this group has also shown that hormone-sensitive lipase (HSL), a key regulator of fat breakdown within fat cells, increases in response to a 3-month endurance exercise training program [16]. With these results, in particular increased HSL protein levels, the article’s authors hypothesized that exercisers may be ‘primed’ for the effective release of fatty acids when stimulated by catecholamines during exercise [1]. Therefore, experiments that investigate a single session of exercise or mimic the conditions of catecholamine-induced fat breakdown within abSAT could test this hypothesis.
Third, direct stimulation of abSAT with insulin could examine the impact of endurance exercise on fat cell insulin sensitivity. Previous research in overfed rodents and adolescent children with obesity suggest that the more rapid inhibition of the fat breakdown in response to low-dose insulin stimulation predicts improved metabolic profiles [22, 23]. The authors note that significant changes to proteins and phosphoproteins involved in fat storage and release were observed among the endurance exercise group. Subsequent studies with a second biopsy or insulin stimulation of fresh abSAT samples would allow researchers to understand the impact of insulin-mediated signaling on fat turnover as it occurs within the body.
Lastly, a previous study from this research group demonstrated that a 3-month endurance exercise training program decreases the size of fat cells within the abSAT [16]. The same study observed other positive adaptations, including increased capillarization, fatty acid regulation, and insulin sensitivity. Although these results occurred in response to a short study duration in which participants were instructed to not lose weight, these findings suggest that the initiation of an endurance exercise training program may help lower the need for abSAT to store lipids due to their utilization as fuel by skeletal muscle. Thus, even without weight loss or gain, abSAT demonstrates rapid plasticity that parallels favorable metabolic responses.
In the recent study, Ahn and colleagues demonstrate another function of endurance exercise - the increased capacity for fat cells to expand and store lipids [1]. It is important to clarify that the subjects in this study were not tracked over a period of time. Instead, fat cells were biopsied from either sedentary or endurance exercisers with obesity at a single time point after their physical activity habits were determined via a questionnaire and differences in fitness levels were determined in the laboratory. In addition, function analysis of fat cells was assessed in a cultured environment for 4 weeks. Therefore, these results do not necessarily reflect a direct measurement of fat cell expansion and storage, but rather their potential to expand if required.
In the future, it would be interesting to examine whether similar changes to abSAT induced by endurance exercise occur in the presence of dietary-induced weight gain. Such a study would provide more direct insight into the potential for abSAT plasticity and its capacity to maintain an adaptive metabolic state among healthy individuals with obesity [24]. Likewise, the identification of an upper threshold or maximal size for fat cell expansion is necessary to determine the upper limits by which endurance exercise preserves metabolic health during obesity.
It is becoming increasingly apparent that abdominal subcutaneous adipose tissue is a major facilitator of metabolic health across the lifespan. Additionally, it is becoming clearer that endurance exercise is a vital behavior that increases the ability of fat cells to be flexible to our current nutritional and metabolic state - decreasing in size when we are in a nutrient deficit and expanding in size during periods of nutrient excess [1, 16]. Indeed, changes to the structure and overall flexibility of fat cells following endurance exercise appears necessary for maintaining metabolic homeostasis and potentially preventing the onset of obesity and age-related disease pathology. As such, these findings highlight the powerful impact of fat cell health and plasticity as a mechanism that contributes to overall healthspan.
TAKE HOME POINTS
Abdominal Subcutaneous Adipose Tissue: Fat stored in the belly region, termed abdominal subcutaneous adipose tissue (abSAT), is a healthy location for fat storage. Its ability to balance fat breakdown (lipolysis) and storage (lipogenesis) highlights a novel mechanism to maintain metabolic health.
Fat Breakdown and Storage: In the fasted state, various hormones stimulate the breakdown of abSAT fat storage to be used as energy. Following food consumption, increased blood glucose concentrations stimulate insulin release by the pancreas. Insulin binds to its receptors in abSAT and rapidly inhibits fat breakdown and increases fat storage.
Complications of Obesity: Obesity is associated with the inability of insulin to inhibit fat breakdown. Excess fats then enter circulation and are stored in areas that surround internal organs and within other tissue types. Fat accumulation in these locations causes whole-body insulin resistance and accelerates age-related disease progression.
Metabolically Healthy Individuals with Obesity: A fraction of individuals with obesity remain insulin sensitive, metabolically healthy, and do not experience the same degree of disease pathology as their insulin-resistant counterparts. The ability of their abSAT to expand and increasingly store fat underpins their metabolic phenotype.
Endurance Exercise Improve abSAT Structure: New research demonstrates that 2-years of habitual endurance exercise training is associated with increased capillary density, decreased extracellular matrix fibrosis, and more favorable macrophage profiles among individuals with obesity compared to their sedentary counterparts with obesity.
Endurance Exercise Improves abSAT Function and Metabolic Health: Improved abSAT structure parallels increased fat cell expansion and storage capacity and increased expression of key genes involved in fat storage (DGAT1 and SREBF1). Likewise, endurance exercisers exhibit improved insulin-mediated glucose uptake and ability to inhibit abSAT fat breakdown compared to sedentary counterparts.
Endurance Exercise Protocol: Consistent participation in endurance exercise for 90 minutes of high-intensity exercise (90% maximal heart rate) or 150 minutes of moderate-intensity exercise (70% maximal heart rate) spread across 3-4 sessions per week (30-45 minutes) appears sufficient for improving fat health.
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.