Clearing out the Cellular Trash: The Importance of Mitophagy in the Removal of Damaged & Dysfunctional Mitochondria
As the lexicon of health, longevity, and anti-aging enthusiasts continues to evolve, one term - 'autophagy' - has solidified its place within the discourse. Nonetheless, a relatively lesser-known offshoot, 'mitophagy,' or mitochondrial-specific autophagy, remains more obscure despite its critical significance. Recent evidence has begun to show how critical this process is in maintaining proteostasis within a cell or tissue and how dysregulation of this process can result in the accumulation of damaged mitochondria.
autophagy
mitophagy
15 mins
By: Dr Ryan N. Marshall, PhD.
Overview
The use of the word 'autophagy' is becoming ever-present in the health, longevity, and anti-aging community. However, the role of mitochondrial-specific autophagy is relatively less understood, termed 'mitophagy.' This process is almost identical to traditional autophagy; however, it focuses solely on targeting damaged, dysfunctional, and ineffective mitochondria for their removal and degradation.
Recent evidence has begun to show how critical this process is in maintaining proteostasis within a cell or tissue and how dysregulation of this process can result in the accumulation of damaged mitochondria, leading to rapid disease progression (Parkinson's, Alzheimer's, T2D, Liver Disease & Muscular Dystrophy).
Here we will discuss some of the exciting recent advances in our understanding of this process and, more importantly, how we can potentially manipulate this with exercise, diet, and pharmacological therapies in an effort to improve cellular health, metabolic health, and longevity.
What is mitophagy?
Mitophagy is a selective process by which damaged or dysfunctional mitochondria are selectively targeted for degradation within cells and is an essential mechanism for maintaining mitochondrial quality control and overall cellular homeostasis [1]. This process involves the engulfment of damaged mitochondria by specialized vesicles called autophagosomes, which then fuse with lysosomes, leading to the degradation and recycling of the targeted mitochondria's contents [1].
Molecular Regulation of Mitophagy & How We Measure This Process
In humans, the process of mitophagy is impossible to directly measure and is limited primarily to snapshots of particular molecular readouts of genes/proteins associated with mitophagy [2]. For example, tissue samples (typically muscle biopsies) from human volunteers, following various interventions, can be analyzed to determine the gene expression or protein abundance of molecular targets such as Pink1, Parkin, P62, LC3B, ULK1 and FUNDC1 [3].
Another side of the mitophagy equation is the molecular machinery that controls mitochondrial dynamics. This is effectively the molecular control of mitochondrial fusion (i.e., the merging of smaller mitochondria to form larger, tubular mitochondria) and mitochondrial fission (i.e., the removal of damaged fragments of mitochondrial to undergo degradation) [4]. These processes are controlled by several proteins, but most notably, OPA-1 [5] & MFN-2 [6], and DRP-1 [7] & FIS-1 [8], which control fusion and fission, respectively.
Unfortunately, these markers, typically assessed via western blot or PCR, only give a snapshot of the time the tissue sample was obtained and do not directly infer mitophagy is occurring. Nevertheless, these indirect and semi-quantitative measures of indirect mitophagy still give us an insight into how this process may be regulated.
A more sophisticated model is the MitoQC (mitochondrial quality control) model developed by Dr Tom McWilliams (now at the University of Helsinki, Finland) and Professor Ian Ganley at The University of Dundee's Protein Phosphorylation Unit [9].
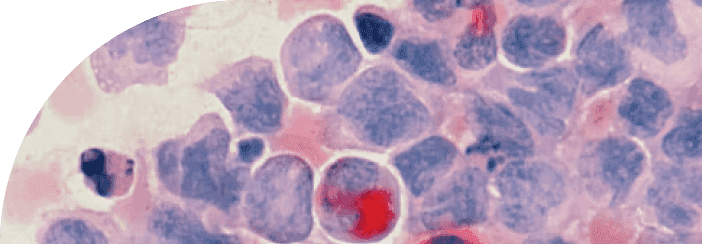
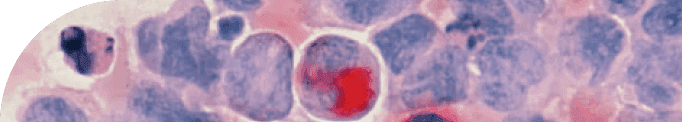
The MitoQC model involves using a fluorescent reporter protein (green fluorescent protein and mCherry) targeted to the outer mitochondrial membrane via the protein FIS-1 [9]. These reporter proteins are designed to accumulate on the mitochondrial membrane under normal conditions within a pH of ~7.2 [10].
However, when mitophagy is induced, the damaged or dysfunctional mitochondria are targeted for degradation via the acidic environment within the lysosome (~pH 4.8), leading to the clearance of the pH-sensitive green fluorescent protein from the mitochondria, resulting in the red puncta of mCherry displaying mitophagy [10].
By monitoring the clearance of the fluorescent reporter protein via a sophisticated confocal microscope and live imaging techniques, researchers can assess the occurrence and efficiency of mitophagy within the cells and tissues at time points or in real time over several hours.
This technique allows for highly sensitive quantitative analysis of mitophagy dynamics. It provides insights into the molecular mechanisms involved in mitochondrial quality control and has been instrumental in advancing our understanding of mitophagy and its regulation.
Can We Manipulate Mitophagy?
Mitochondrial dysfunction has been implicated as one of the nine hallmarks of aging, along with other hallmarks such as epigenetic alterations, genomic instability, cellular senescence, stell cell exhaustion, telomere attrition, dysregulated nutrient sensing, loss of proteostasis and altered intracellular communication [11].
Mitochondrial dysfunction can be subcategorized into decreased mitochondrial biogenesis, decreased respiratory capacity, increased ROS production, a decline in mitochondrial content, and impairments in mitochondrial quality control and removal of damaged/dysfunctional mitochondria via mitophagy [12].
Emerging evidence suggests that enhancing mitophagy can positively impact longevity and lifespan. Several studies involving genetic mutation, dietary manipulations, or pharmacological interventions have demonstrated that promoting mitophagy extends the lifespan in various model organisms, including yeast [13], worms [14], flies, and mice [15].
Moreover, impaired mitophagy has been linked to age-related diseases, such as neurodegenerative disorders [16] and cardiovascular disease [17]. Dysfunction in mitophagy pathways can lead to the accumulation of damaged mitochondria, oxidative stress, and inflammation, contributing to the pathogenesis of these diseases.
Enhancing mitophagy through pharmacological interventions or lifestyle modifications holds promise for mitigating age-related diseases and promoting healthy aging. Here we will briefly discuss how exercise, nutrition, and pharmacological interventions can improve mitophagic regulation, improve mitochondrial quality control as we age, and prevent the accumulation of damaged mitochondria within cells & tissues.
Exercise and Mitophagy
The effect of exercise, particularly endurance/HIIT exercise, has significant evidence regarding its impact on mitochondrial biogenesis and mitochondrial respiration, resulting in improved health [18] and increased exercise performance [19].
Until recently, the role of exercise & mitophagy was relatively unclear. In 2017 and 2020, two post-doctoral researchers in the laboratory of Professor Zhen Yan at the University of Virginia's Centre for Skeletal Muscle Research published incredible work displaying the role of exercise on muscle mitophagy.
The first, Dr. Rhianna Laker (now a Research Scientist & Team Leader at AstraZeneca), showed (in mice) that 90 minutes of treadmill running induced a 45% increase in mitophagy (i.e., green:red ratio) [20].

Mitophagy
Using a similar reporter model (MitoTimer) [21], we can see how exercise results in the fluorescent color change 6hrs post-exercise. Notably, there was a >400% increase in the number of pure red fluorescent puncta in the fibers, indicating significantly elevated levels of mitochondria being degraded via the lysosome [20].
In this study, the group displayed that mitophagy is preceded by the phosphorylation of AMPK and its downstream target, ULK-1. To confirm AMPK's role in mitophagy, the authors used a mouse model to knock out the dominant α2 subunit of AMPK and subjected the mice to the same exercise. Following 90 minutes of treadmill exercise, no mitophagy was detected [20].
Secondly, a follow-up to this by Dr Joshua Drake (now an assistant professor at Virginia Tech) showed the crucial role of AMPK in mitophagy [22]. For the first time, he and the team showed that AMPK is actually localized to the mitochondrial membrane following exercise or energetic stress.
Within this study, the team tested the hypothesis of metformin, a method of inducing energetic stress and thereby increasing mitophagy. Metformin directly impaired complex I, as previously reported, with little to no effect on mitochondrial respiration [22]. However, as previously reported with exercise, metformin increased mitochondrial localized AMPK [22], indicating the potential for metformin to induce skeletal muscle mitophagy independent of exercise.
Adenosine monophosphate-activated protein kinase (AMPK) is an enzyme that plays a crucial role in cellular energy homeostasis and metabolism. When cellular energy levels are low, such as during nutrient deprivation, exercise, or stress conditions, AMPK becomes activated. This activation occurs through a mechanism where AMP binds to the regulatory subunits of AMPK, leading to phosphorylation of the catalytic subunit by upstream kinases. Once activated, AMPK initiates a series of responses to restore energy balance within the cell and maintain cellular viability.
Nutrition and Mitophagy
The world-leading laboratory of Professor Johan Auwerx at the École Polytechnique Fédérale in Lausanne, Switzerland, have collaborated with Amazentis (a Nestle Health Science company) on the development and now commercialization of a nutritional supplement aimed at improving mitophagy.
This collaboration has earned the team several high-profile publications in Nature Metabolism, Nature Medicine, and JAMA. The translation research process from cells to c.elegans (worms), mice and even humans have consistently observed improvements in mitochondrial health and, notably, increased mitophagy.
The active ingredient behind the success is an extract from pomegranate called 'Urolithin A'. This ingredient has since been patented by Amazentis and commercialized as a 'mitophagy activator' supplement under the brand name 'mitopure'.
"Urolithin A is a metabolite that is produced in the human body from ellagitannins, which are a type of polyphenol found in various fruits and nuts, in particular pomegranates, strawberries, raspberries, and walnuts."
What is interesting about natural Urolithin A is how it is synthesized. The process is incredibly variable and only occurs in approximately 40% of the human population [23], hence why supplementation is essential to elevate blood concentration [24]. Being a 'UA responder requires the appropriate gut microbiome, and in particular, bacteria species, Gordonibacter urolithinfaciens and Ellagibacter isourolithinifaciens, which convert the ellagitannins from pomegranates and other sources into active Urolithin A [24].
Initial evidence in 2016 from Professor Auwerx's lab and the start of the Amazentis Urolithin A research showed this nutritional supplement increased lifespan in c.elegans by 45%, which was primarily due to improved mitochondrial function [25].
"C. elegans are a small, transparent roundworm used as a model organism. Its short lifespan, quick reproduction, invariant cell lineage, and genetic similarities to humans make it valuable for studying development, genetics, aging, and diseases in a simple and easily maintained laboratory setting."
To explore this further, the authors determine with a sensitive reporter model of mitophagy (termed 'MitoKeima' – A similar model to MitoQC). Following a 24hr exposure to Urolithin A in muscle cells, mitophagy was increased by ~104% compared to control [25]. In mice [25], middle-aged adults [26], and older adults [27], Urolithin A has been observed to increase the gene & protein expression of proteins related to mitophagy.
Data from randomized control trials of middle-aged adults supplementing 1,000mg/day for 4 months reported improvements in muscle strength (~12%) and endurance performance (~12%). Muscle biopsies obtained pre & post-intervention from the vastus lateralis muscle of the quadriceps showed a significant increase in genes related to mitophagy, TCA cycle, and fatty acid oxidation, overall indicating improvements in mitochondrial health & function [26].
Pharmacological-Induced Mitophagy
It's well established that Rapamycin induces autophagy by suppressing mTOR activity. Therefore, it should likely have an effect on mitochondrial-specific autophagy, right?
Surprisingly, there's not too much evidence on the effects of Rapamycin on mitophagy. However, a recent 2022 paper published in Cell Metabolism by Dr Tom McWilliams has characterized the role of Rapamycin in mitophagy in a model of mitochondrial disease using the previously mentioned reporter models, which he developed during his PhD [28]. This model has some similarities to aging, in which older adults, especially octogenarians >80yrs age, display severe mitochondrial abnormalities [29].
The study shines light on the role of this powerful drug on mitochondrial quality control. The model of mitochondrial disease typically displays respiratory chain defects, 'ragged-red fibers' (expressing pathogenic mitochondria DNA variants & severe accumulation of damaged mitochondria) [28].
This study showed that the treatment of Rapamycin at a dose of 8mg/kg/day for 70 days resulted in a 125% increase in mitophagy [28]. The authors speculated that in aging and mitochondrial disease, there's hyperactivation of autophagy-mediated degradation as indicated by the accumulation of P62 and phosphorylated ubiquitin in muscle fibres [28]. Notably, compared to healthy control patient samples, patients with mitochondrial disease displayed an >80-fold increase in the autophagy adapter protein P62, with rapamycin treatment causing a ~90% decrease in the hyper-autophagy state and restoring it to 'normal' levels [28].
Digging into the supplementary data within the publication, the authors state that one of the mechanisms of action in improved mitophagy is likely due to the decrease in phosphorylated s6, a downstream marker of mTOR activity [28].
In the 20 years from 1999-2019, there has been an increased prevalence of Alzheimer's, with >6 million adults aged >60 suffering from the disease. Although there is a genetic component to this disease via the APO-e4 gene, changes to dietary, exercise, and other environmental influences may accelerate its progression.
"The ApoE4 gene, also known as the apolipoprotein E4 gene, refers to a specific variant of the apolipoprotein E (APOE) gene. APOE is a gene that provides instructions for producing a protein called apolipoprotein E, which plays a crucial role in lipid metabolism. The APOE gene has three common variants: APOE2, APOE3, and APOE4. The E4 variant is associated with an increased risk of developing neurodegenerative disorders. The APOE4 gene has been identified as a major genetic risk factor for late-onset Alzheimer's disease".
Since 2019, Professor Matt Kaeberlein has been calling for clinical trials into Rapamycin as a therapeutic tool to prevent and slow Alzheimer's disease. He even wrote an article published in Science Translation Medicine titled "Rapamycin and Alzheimer's disease: Time for a clinical trial?" [30].
This drug has a compelling pre-clinical record in mice showing outstanding benefits, including reducing amyloid-β(Aβ) deposition, reducing pathogenic tau phosphorylation and abundance of misfolded tau species, including neurofibrillary tangles, restoring cerebral blood flow, preserving blood-brain barrier integrity, and improving cognitive function [30].
In a model of Alzheimer's, the potential of the mitochondrial membrane decreases and the permeability increases, which leads to increases in ROS production and cytochrome C release, eventually inducing neuronal apoptosis.
Recent studies have begun to explore the molecular processes by which Rapamycin alters brain metabolism, with mitochondrial function and particular mitophagy and quality control (i.e., the synthesis of new mitochondria and subsequent degradation of old/damaged mitochondria) playing a critical role.
In aged mice, the treatment with Rapamycin increases mitochondrial protein synthesis (i.e., biogenesis & building of new mitochondria). Utilizing state-of-the-art stable isotope tracer techniques, Professor Benjamin Miller's research group at Oklahoma Medical Research Foundation has observed no effect of Rapamycin on brain mitochondrial protein synthesis in younger mice 31.
However, in an older cohort, Rapamycin induced a nearly 40% increase in mitochondrial protein synthesis, with no distinct effect on mTOR, AMPK, or protein aggregates (i.e., insoluble amyloid-beta plaques (Aβ) and neurofibrillary tangles of tau protein) [31].
"Stable isotope tracer techniques are powerful tools used in scientific research, specifically in the field of protein synthesis. These techniques involve the use of stable isotopes, which are non-radioactive forms of elements (typically carbon-13 (13C), nitrogen-15 (15N), and deuterium (2H), to track and measure the metabolic processes related to protein synthesis in living organisms."
On the other side of mitochondrial quality control, others have sought to determine how Rapamycin can force the removal of damaged/dysfunctional mitochondria within the aging brain. Although no research group to date has used the powerful Mito-QC model to study mitophagy dynamics, several authors have probed the effects of Rapamycin on molecular markers associated with mitophagy in models of Alzheimer's [32].
An 8-week study of daily Rapamycin (1mg/kg/day) enhanced learning and memory, synaptic plasticity, and the expression of synapse-related proteins [32]. Although not as sensitive as the Mito-QC model, the authors attempted to determine how autophagy proteins co-localize in an attempt to quantify mitophagy.
In this method, they chose to assess the co-localization of TOM20 (an outer mitochondrial membrane protein) & LC3B (a key marker of the autophagosome), in which greater co-localization translates to increased mitochondrial-specific mitophagy. Rapamycin treatment increased mitophagy by >400% compared to the non-treatment group, which was concurrent with an increase in the protein expression of P62, Parkin and LC3B within the mitochondrial fraction of the brain. This is a crucial step to isolate the mitochondria during analysis, as the whole-brain tissue sampled in this study actually observed a decline in mitophagy-related markers [32].
What does this all mean?
Imagine your body's cells as a bustling city, with each cell serving as a home to a multitude of mitochondria. Over time, some of these mitochondria become damaged or dysfunctional, much like waste accumulating in a city. But fear not, for your body has a team of diligent garbage men called mitophagy, ready to clear out the cellular trash.
Just like garbage collectors roam the streets, mitophagy patrols the inner workings of your cells, identifying and targeting those dysfunctional mitochondria for removal. They possess specialized tools and mechanisms to distinguish the good from the bad, much like how trained eyes can distinguish recyclables from general waste.
When a mitochondrion becomes damaged, it displays molecular signals. These signals act as a beacon, attracting the attention of the mitophagy crew. Once identified, the garbage men surround the damaged mitochondrion, enclosing it in a specialized membrane, similar to placing a hazardous waste bag around a bin.
With precision and efficiency, the mitophagy team then proceeds to engulf the damaged mitochondrion within a double-membrane structure, resembling a garbage truck devouring its contents. This structure, called an autophagosome, safely engulfs the malfunctioning mitochondrion, isolating it from the healthy ones.
Just like a garbage truck transporting its load to a waste processing facility, the autophagosome transports the captured mitochondrion to a cellular recycling center called the lysosome. The lysosome acts as a cellular incinerator, breaking down the damaged mitochondrion into its component parts, recycling valuable materials, and disposing of waste products.
In this process, mitophagy acts as the tireless garbage men, diligently patrolling your cells, identifying, and removing damaged mitochondria to maintain a clean and functional cellular environment.
By eliminating dysfunctional mitochondria, mitophagy helps prevent the accumulation of cellular waste, reducing the risk of oxidative damage and maintaining overall cellular health, much like efficient waste management contributes to a cleaner and healthier city.
Just as we rely on the dedication of garbage collectors to keep our cities clean and liveable, our bodies depend on the vigilant work of mitophagy to ensure the efficient removal of damaged mitochondria and maintain cellular well-being. So, next time you see a garbage truck passing by, remember the incredible parallel of mitophagy, tirelessly working to keep your cells free from the waste of dysfunctional mitochondria.
TAKE HOME POINTS
Mitophagy is essentially mitochondrial-specific autophagy.
Measuring mitophagy in humans is currently impossible, but mouse models allow us to measure this process in incredible detail.
Exercise induces large increases in mitophagy process but returns to baseline levels ~24hrs post-exercise. Therefore, repeated bouts of exercise, either daily or as many times per week, are essential to maintain healthy mitochondria and remove the damaged & dysfunctional ones.
Nutritional supplements, in particular Urolithin A, can increase mitophagy, and improve mitochondrial health independent of exercise. However, a direct study of exercise + Urolithin A/Placebo is likely needed to determine its true effect on mitophagy compared to exercise.
Rapamycin has been shown to induce autophagy via decreased mTOR activity. New research is showing this also has a beneficial effect on mitophagy and can have a beneficial effect on brain mitochondria via the synthesis and biogenesis of new mitochondria, as well as the clearance of damaged & dysfunction mitochondria through mitophagy. Overall, this may treat, offset, or at least slow down the progression of neurodegenerative diseases such as Alzheimer's.
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.