Muscles, Memory, and the Aging Brain: A Story of Two Systems
Every three seconds, someone in the world develops dementia—a statistic that underscores the urgency of understanding its underlying causes and potential preventive strategies. While dementia is often approached as a brain-centered disorder, emerging research suggests that the condition of our muscles may play a more central role than previously recognized. Sarcopenia, the age-related loss of skeletal muscle mass and function, has long been associated with physical decline in older adults. However, its potential impact on cognitive health is only beginning to be understood. This review examines findings from a longitudinal study led by Dr. Stephanie Chevalier and colleagues at McGill University, using data from the Canadian Longitudinal Study on Aging. The researchers tracked changes in appendicular lean mass and cognitive function over three years in a cohort of community-dwelling adults. Their results reveal notable associations between low muscle mass and declines in memory, executive function, and psychomotor speed. We also explore the biological mechanisms that may connect muscle and brain health, particularly the role of muscle-derived signaling molecules such as brain-derived neurotrophic factor (BDNF), interleukin-6 (IL-6), and insulin-like growth factor-1 (IGF-1). These myokines offer a compelling framework for the emerging concept of the muscle-brain axis, where muscle tissue acts not only as a mechanical system but also as an endocrine organ influencing cognitive resilience.
22 mins
By: Dr. Jennifer Szu
Introduction
Changes in cognitive function, such as a gradual decline in memory or slower processing of new information, are a normal part of aging. However, the transition from normal aging to dementia is increasing globally. According to Alzheimer’s Disease International, over 55 million people worldwide were living with dementia in 2020, and this number is projected to double every 20 years. The staggering prevalence of dementia with age negatively impacts both the quality of life for the patients and their families. Shockingly, the economic and societal burden of dementia, particularly Alzheimer’s disease, is astounding, with a global cost of dementia currently above USD 1.3 trillion and is expected to surge to USD 2.8 trillion by 20301.
Dementia is a broad term that encompasses various types of dementia. The most well-known type of dementia is Alzheimer’s disease. Other categories of dementia include vascular dementia, Huntington’s disease, Parkinson’s disease, Creutzfeldt-Jakob disease, amongst others2. There are also different stages of dementia. Earlier stages of dementia include exhibiting symptoms such as not being able to recall names or getting lost while driving. Individuals with severe dementia have marked impediments in memory functions and may be incapable of communicating, walking, or eating3.
Sadly, dementia is irreversible, and there are currently no successful therapeutic options. Specifically, treatments for Alzheimer’s disease have consistently failed, and many drugs in clinical trials have not been successful in reaching their goals. While there may potentially be no possible way yet to prevent cognitive decline therapeutically, there are certain measures that one can take to slow down the progression of dementia. Numerous studies connect muscle mass with cognition, where loss of muscle mass is associated with cognitive impairments. Therefore, physical exercise has emerged as a non-pharmacological method to improve brain health. Indeed, mounting evidence exists on the positive effects that physical exercise exerts on mental performance4-6.
Sarcopenia is the progressive degeneration of skeletal muscle mass, strength, and function, typically associated with aging. Sarcopenia is formally recognized as an official muscle disease7 and affects 10 – 16% of the elderly worldwide8. This prevalence is higher in patients with health disorders such as diabetes and cancer. The loss of muscle mass and function is particularly concerning in the older population as it is commonly the cause of falls, weakness, and even death. This condition involves the deterioration of both the quality and quantity of skeletal muscle. Factors contributing to sarcopenia include heightened inflammation, environmental stressors, loss of motor neurons, and decline in activity and nutrition8. Therefore, improving and enhancing muscle mass and function in older people improves physical and mental fitness.
In a 2022 paper published by Dr. Stephanie Chevalier and her team from McGill University, the authors found a correlation between low appendicular lean soft tissue mass (ALM, proxy for skeletal muscle mass) and cognition in the aging population. The Canadian Longitudinal Study on Aging is a prospective study to determine whether low muscle mass in older community-dwelling adults is associated with declines in different cognitive domains over 3 years 9.
Study population
Study participants were enrolled between 2011 and 2015, including 30,097 males and females. This study evaluated the association between ALM and cognition in 8279 participants (4003 or 48% female and 8005 or 97% male) with a median age of 72.9 (5.6 years). The participants could speak English or French and had no cognitive impairments at the time of recruitment. Participants with clinical conditions (such as Alzheimer’s disease, Parkinson's disease, those who received chemotherapy, traumatic brain injury, etc.) that may impact the outcome of the study were excluded from the study.
Neuropsychological assessment
Clinical assessments at baseline and 3-year follow-up included the following neuropsychological tests, which examined three discrete cognitive domains:
1. Memory: Immediate and verbal learning were tested using the 15-word Rey auditory-verbal-learning test (RAVLT). The RAVLT test involves giving participants a list of 15 words and then asking them to recall as many words as possible. A second 15-word list and a recall of the first list follow this. In this study, the authors used results of the first trial (immediate recall) and results of the second trial (5-minute delayed recall).
2. Executive functions: Executive function is a collection of mental skills used to manage everyday tasks, including attention, control, and working memory. In this study, four tests were employed to test for executive function:
Mental-alternation test (MAT): Measures cognitive flexibility and working memory by having participants alternate between two sequences as quickly and accurately as possible (eg, switching between numbers and letters).
High interference (color names in incongruent colors/colored dots) of the Stroop test: Evaluates cognitive inhibition by having participants name the color of the ink in which a word is printed (eg, the word “yellow” printed in the color blue).
Animal-fluency test (AFT): Consists of naming as many animals as possible in a short period.
Controlled-oral-word-association test for the letters F, A, and S (COWAT): A verbal fluency test where participants say as many words as possible that start with F, A, and S for 60 seconds.
3. Psychomotor speed: Assessed using computer-administered choice reaction times.
Body composition
Whole body composition was measured at baseline using dual-energy x-ray absorptiometry (DXA or DEXA), and ALM was defined as having at least 95% skeletal muscle. As set by the Canadian cut points for low ALM index, Sarcopenia was defined as10: for males < 7.30 kg/m2 and females < 5.42 kg/m2. Additionally, sociodemographic and lifestyle characteristics were collected at baseline based on phone interviews or in person.
Other covariates
During baseline, demographic and lifestyle characteristics were also collected by phone or in person. Demographic data included sex, language, level of education, household income, and ethnicity. Lifestyle characteristics included cigarette smoking, alcohol use, and social participation. Other covariates included symptoms of depression, level of physical activity, nutrition, and health. Grip strength was also evaluated using a handheld dynamometer, where the highest value of 3 trials was used in analyses.
Baseline measurements
At baseline, 1605 (19.4%) of participants had low ALM. Low ALM was observed mostly in older men who were current daily smokers. Additionally, participants with low ALM exhibited lower BMI and less physical activity. Individuals with low ALM also had significantly poorer memory performance, lower executive function, and worse psychomotor speed than those without low ALM.
Findings after 3-year follow-up:
1. Memory:
Improved in the immediate (0.4, p < 0.001) and delayed recall (0.3, p < 0.001). This finding indicates that, overall, after 3 years, participants were able to significantly increase the average number of words they could immediately recall (trial 1) by 0.4 words. Additionally, participants had an average gain of 0.3 words in the delayed recall (trial 2).
Participants with low ALM exhibited a lesser increase in immediate recall compared to those without low ALM (0.3 vs 0.4, p = 0.04). These findings demonstrate that participants without low skeletal mass could recall significantly more words than those with low skeletal mass by an average of 0.4 words compared to 0.3 words, respectively.
2. Executive function:
Decreased performance in animal naming, the MAT test, and Stroop high interference. Participants with low ALM had a greater reduction in animal naming (-0.6 vs -0.3, p = 0.1) and MAT test scores (-1.4 vs -0.9, p = 0.008). After 3 years, participants with low ALM had an overall decrease in the total number of unique animal names they could recall (average of -0.6 words) compared to participants without low ALM (average of -0.3 words). However, this was not statistically significant.
COWAT total score was improved; however, participants with low ALM still exhibited a decrease in the COWAT score compared to those without low ALM (-0.1 vs 0.5; p = 0.04). These findings found that the number of words the participants were able to produce for the COWAT test improved after 3 years. However, participants with low ALM still displayed a decrease in their score (average -0.1 words produced) compared to those without low skeletal mass (average 0.5 words produced). These findings suggest that participants without low ALM significantly improved their ability to create unique words.
3. Psychomotor speed:
No statistically significant changes were observed.
Participants with low ALM have a greater decline in executive function
Executive functions rely on cognitive skills essential for managing everyday tasks, including working memory, mental flexibility, and inhibition control11. In this study, the authors found that participants with low ALM exhibited a greater decline in executive function, independent of all covariates, including physical activity and grip strength. This finding suggests that sarcopenia, or loss of muscle mass and function, is the primary predictor for the decline in executive function in the aging population, rather than merely a reflection of reduced physical exercise or muscular strength. This is an interesting finding as muscle mass, strength, and physical activity tend to have a positive correlation; however, this is not always linear. Indeed, prior studies have found that muscle weakness in older individuals is primarily due to loss of muscle quality rather than loss of muscle mass12.
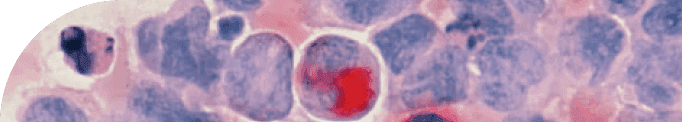
Muscle quality comprises both the structural and functional aspects of the muscle. Functional characteristics of the muscle mainly include the force, strength, and power of the muscle (ie, muscle performance)13. The structural or architectural component of the muscle lays the foundation for muscle quality. It consists primarily of muscle fibers and less of the connective tissue and fat between and around the muscles12. Increases in the fat within the muscle, also known as intermuscular fat or intermuscular adipose tissue (IMAT), reduce muscle quality and function and lead to negative consequences such as chronic inflammation, increased cholesterol, and impaired glucose tolerance12,14.
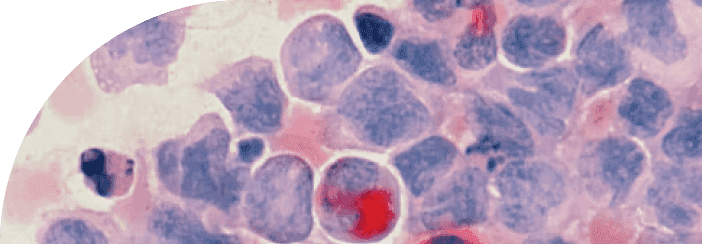
Skeletal muscles are muscles that attach to bones, are involved in our daily movement patterns, and are under voluntary control. Skeletal muscle fiber consists of type 1 and type 2 fibers. Type 1 is also known as “slow twitch,” where it has a slow contraction speed and is highly resistant to fatigue. These muscle fibers are more suited for aerobic activities. Type 2 is known as “fast twitch,” where it contracts quickly but experiences rapid fatigue. These muscle fibers are best utilized for short bursts of activity, but also tend to achieve more muscle growth through exercises such as strength training12. Studies have found that a decline in type 2 muscle fibers is associated with aging and contributes to sarcopenia15.
It is important to note that regular physical activity or exercise plays a crucial role in muscle quality and overall muscle mass. Prior studies have shown that simple aerobic exercises like walking can improve skeletal muscle quality and quadriceps strength16. In the study reviewed here, participants with low ALM engaged in less physical activity at baseline than those without ALM. They experienced worse neuropsychological outcomes (memory performance, executive function, and psychomotor speed). This reinforces the many studies demonstrating that regular exercise, particularly strength or resistance training, can improve muscle quality and preserve muscle mass to ultimately maintain cognitive functions.
It is unknown what changes the participants have made to their physical health over the 3 years that led to the unexpected finding of improved memory. While memory loss is generally associated with aging, there may be certain concerns with how the tests were administered that may have impacted the outcomes. For example, while the RAVLT test is sensitive for measuring cognitive impairments, there may be a retest effect. In other words, as participants become more familiar with the test, they can perform better, not because their memory has improved. Additionally, time-saving modifications in the RAVLT test (1 trial vs 5 in the original test and 5-minute vs 30-minute delay) may have also influenced the reliability of detecting memory deficits. Thus, the overall improvements in memory after 3 years may have concealed actual cognitive decline that the participants may be experiencing. Nevertheless, what is obvious is that low muscle mass is a key indicator of overall cognitive performance as displayed by the loss of executive function. Core executive function integrates fundamental cognitive processes to support goal-directed behavior and decision making, and the loss of skeletal muscle correlates with the decline in these abilities.
Myokines at the center of the muscle-brain axis
There is growing evidence linking sarcopenia to cognitive decline, with research also highlighting that physical activity can improve brain function and overall cognitive health. Physical activity or exercise is connected with the brain via the muscle-brain axis. The muscle-brain axis is a two-way communication between the skeletal muscle and the central nervous system (CNS), which includes the brain and the spinal cord. The muscle-brain axis is activated through myokines, molecules secreted by skeletal muscles during physical exertion (muscular contractions), and exhibits autocrine, endocrine, and paracrine functions17. Importantly, myokines have been shown to potentiate positive brain effects such as neuroprotection, anti-inflammatory properties, metabolism, and muscle and bone health.
Currently, over 3000 myokines have been identified18. Below are three examples of exercise-induced myokines that play a central role in cognition:
BDNF
Brain-derived neurotrophic factor (BDNF) is a molecule that is critically involved in learning and memory and is found primarily in the cortex and the hippocampus of the brain. BDNF promotes neuronal growth and regulates synaptic plasticity, the ability of the brain to strengthen or weaken connections, and is a key mechanism underlying learning and memory19. Studies have found that aerobic exercise enhances BDNF expression in the hippocampus, ultimately increasing neurogenesis (creating new brain cells). Furthermore, BDNF is involved in long-term potentiation, a form of synaptic plasticity, and is the cellular correlate of memory formation20. Therefore, increased levels of BDNF derived from skeletal muscles after physical exercise are one mechanism for improving learning and memory.
Hippocampal loss or deterioration is known to precede memory loss and is observed in the aging population. Aerobic exercise has been shown to increase the volume of the brain's gray and white matter, reducing the risk of cognitive deficits. In an early study by Erickson et al., the authors found that aerobic exercise in 120 older adults increased the size of the hippocampus (neurogenesis), resulting in improved spatial memory. Impressively, aerobic training enhanced the hippocampal volume by 2% and reversed age-related volume loss by 1 – 2 years. Not surprisingly, the increased BDNF levels found associated with exercise further support the role of BDNF in enhancing neurogenesis in the hippocampus and improving memory21.
The hallmarks of Alzheimer’s disease are characterized by 1) the accumulation of toxic amyloid plaques, clumps of proteins composed of amyloid beta, and 2) neurofibrillary tangles, which are aggregates of twisted strands of tau proteins that become hyperphosphorylated (over-modified tau proteins). These biological markers disrupt normal cellular communication, increase neuroinflammation, impair memory function, and ultimately result in cell death22. Interestingly, reductions in BDNF have been detected in post-mortem brains of Alzheimer’s patients and mouse models of Alzheimer’s disease, suggesting that BDNF may play a neuroprotective role against neurotoxicity induced by Alzheimer’s disease pathophysiology. Mouse models of Alzheimer’s disease found that consistent endurance exercise reduced the levels of hyperphosphorylation of tau proteins as well as decreased the deposition of amyloid plaques in the brain. This may be attributed to increased BDNF after exercise, which reduced neuroinflammation and ameliorated spatial and learning deficits23. These findings show that physical exercise can reduce the risk of developing dementia and Alzheimer’s disease by increasing BDNF.
IL-6
Interleukin-6 (IL-6) is most commonly known as a pro-inflammatory cytokine, where it displays an inverse relationship with cognitive function. Studies have found that enhanced levels of IL-6 have been shown to correlate with poor cognitive performance and negatively impact learning and memory. IL-6 also affects the pathophysiology of Alzheimer’s disease. IL-6 is associated with early-stage amyloid plaque formation, phosphorylation of tau, loss of synapses, and impaired learning. Indeed, high plasma levels of IL-6 have been found in post-mortem Alzheimer’s disease brains, which were positively correlated with cognitive deficits24. Moreover, elevated levels of IL-6 can also lead to structural damage to the brain, specifically reducing hippocampal volume, white matter loss, and increasing neurodegeneration, all of which contribute to the risk of dementia onset25,26.
While increasing IL-6 levels may have negative effects on brain health, decreased baseline or resting levels of IL-6 have been shown to promote a neuroprotective role after regular exercise. Firstly, levels of plasma IL-6 after exercise are dependent on the type and duration of exercise. Studies have determined that levels of IL-6 rise sharply temporarily following exercise or prolonged high-intensity physical activity. Additionally, research has shown that plasma IL-6 increases significantly as a function of exercise duration. The greatest increase in IL-6 concentrations was reported after a 246 km foot race, while most exercises less than an hour do not induce such a marked increase in IL-6. Moreover, high intensity exercise with subsequent increased %VO2max (maximum amount of oxygen your body consumes during intense exercise) was also significantly correlated with increased IL-6. Increased levels of plasma IL-6 were not observed in short-duration exercises with lower %VO2max 27. Elevated chronic levels of IL-6 have been shown to contribute to muscle atrophy and disrupt muscle growth, which may result from high-intensity or prolonged exercise.
On the contrary, regular exercise reduces the resting levels of IL-6, which may promote an anti-inflammatory effect. Indeed, moderate-intensity and strength training in the elderly population increased muscle strength and stability and decreased the levels of IL-627. The reduction in IL-6 levels after regular aerobic or resistance exercise exhibits anti-inflammatory properties and can also regulate immunosenescence, changes in the immune system associated with aging. Thus, physical activity may mediate a neuroprotective role against inflammation and ultimately improve functions such as working memory, processing speed, and attentional processes.
IGF-1
Normal aging correlates with the decline of insulin-like growth factor 1 (IGF-1), a peptide hormone secreted primarily from the liver but can also be synthesized in a paracrine manner. Increased peripheral levels of IGF-1 after exercise have been shown to have positive impacts on cognitive performance. Prior studies in the elderly population found that high levels of serum IGF-1 were associated with improved cognitive function, while those with cognitive impairments had lower levels of IGF-1. Furthermore, physical exercises such as aerobic and resistance training in older adults were found to not only increase IGF-1 but also maintain IGF-1 levels. This correlated with improved cognitive training, such as RAVLT, German Weschler Adult Intelligence Scale, Stroop test, amongst others28.
IGF-1 has also been shown to play important roles in learning and spatial memory. In a preclinical study, rats underwent 8 weeks of either aerobic (treadmill) or resistance (vertical ladder) training. In both groups, increased levels of IGF-1 and BDNF were observed in the hippocampus, a key part of the brain that is important for memory formation. Moreover, the animals that underwent resistance training displayed significant increases in IGF-1R, indicating the activation of its downstream signaling survival pathway (IGF1/PI3K/Akt). This signaling pathway activation increased synapsin and synaptophysin expression, proteins critical for synaptic plasticity.
Furthermore, rats with physical activity training had improved spatial memory as evaluated by the Morris water maze compared to those that did not29. In a separate study, aging-induced rats displayed a reduction in the IGF1/PI3K/Akt pathway. Interestingly, swimming exercise in these aging rats enhanced and stimulated the IGF1/PI3K/Akt pathway and reduced levels of brain apoptosis (cell death) and inflammatory signaling 30. These findings emphasize the crucial role of physical exercise in improving cognitive health through the induction of IGF-1 as well as reducing age-related pathological changes in the brain.
Since myokines are central to the connection between muscle mass and cognitive decline, it can be deduced that dysfunction in myokine signaling is one pathophysiological mechanism underlying cognitive impairments in the older population. As previously mentioned, thousands of myokines have been identified, and each plays a pivotal role in cognitive performance and overall health. Myokines also play a role in inflammation (as discussed with IL-6), metabolism, and mitochondrial function, among others. Although discussion around the many plausible mechanisms underlying deficits in myokine communication via the brain-muscle axis is beyond the scope of this review article, what is evident is the necessity of engaging in regular physical activity to promote muscle mass and function to protect from potential cognitive decline as we age.
Aerobic and resistance training on muscle mass in the elderly
Aerobic and resistance or strength training have frequently been mentioned as the physical activity of choice in the older population to improve cognitive functions. But what exactly is aerobic and resistance or strength training, and what are its effects on muscle mass?
Aerobic exercise: According to the World Health Organization, aerobic exercise is an activity that involves the body’s large muscles moving in a sustained period where oxygen demand does not surpass oxygen supply. Aerobic activity is commonly called “cardio,” and cardio activities use oxygen to fuel muscles. Examples of aerobic exercise include walking, running, swimming, and bicycling.
Aerobic exercise has tremendous effects on overall health, such as improving cardiovascular fitness and endurance. However, while moderate aerobic exercise may not increase skeletal muscle mass, studies demonstrated that regular treadmill walking for 12 – 24 weeks at intensities between 50 – 75% VO2peak can preserve muscle mass 31. Prior research has also shown that lifelong aerobic athletes can preserve muscle mass and function with age32. Studies found that high-level recreational athletes, aged 40 – 81 years old, maintained their muscle mass and muscle strength and prevented fat accumulation in the muscle33. In a separate study, lifelong aerobic exercise decreased fat infiltration by 50% in both men and women over 70 years old34, further emphasizing the importance of regular aerobic exercise to delay the onset of age-related chronic diseases.
Resistance or strength training: This physical activity involves resistance to muscular contraction to build strength and anaerobic endurance. Resistance or strength training is typically achieved using weights (such as dumbbells or barbells) but can also include body weight.
A wealth of evidence indicates that resistance exercise training in older adults can significantly increase muscle mass and function35,36. Remarkably, resistance training is the most common exercise that can prevent and/or delay sarcopenia in older adults, specifically by improving type 2 muscle fiber37. In a meta-analysis of sarcopenic older individuals over the age of 60 years, resistance training and mixed training (combined with other exercises that focus on balance, endurance, and aerobic) improved muscle strength and walking speed38. In one study, 16 weeks of resistance training significantly improved muscle quality in sarcopenic women over 65. Grip strength significantly improved from 20.8 ± 2.93 at baseline to 24.3 ± 2.25 kg after the 16-week resistance training period. Gait speed also significantly improved after resistance training, from 0.96 ± 0.08 to 1.14 ± 0.11 m·s-1 39. In a separate study, 12 weeks of progressive whole-body resistance training improved ALM and muscle strength in individuals between the ages of 65 – 75 years and those over 85+ years40. These findings highlight the significance of resistance training in older adults to combat sarcopenia and improve overall health.
The findings published by Chevalier and her team proposed that low ALM was the greatest predictor of decline in executive function. These results stress the need for older individuals to engage in regular physical activity, particularly aerobic and resistance training, to maintain muscle mass and quality and preserve or maintain cognitive functions.
Physical activity recommendations for older adults
Given that loss of muscle mass is correlated with a decline in cognition, it is imperative to engage in physical activity to battle degradation in brain function as we age. The World Health Organization monitors trends in physical activity and found that physical inactivity declines after 60 years of age and that women are less active than men. Below are the WHO’s recommendations on physical activity for older adults ≥ 65 years of age:
Engage in at least 150 – 300 minutes of moderate intensity aerobic physical activity or at least 75 – 150 minutes of vigorous intensity aerobic physical activity. For additional health benefits, the duration of these exercises can be increased (eg, more than 300 minutes of moderate intensity aerobic physical activity or more than 150 minutes of vigorous intensity aerobic physical activity).
Perform moderate or greater-intensity muscle strengthening activities involving all major muscle groups for at least 2 days a week.
Include a varied multicomponent physical activity that emphasizes functional balance and strength training at moderate or greater intensity for at least 3 days a week.
Conclusions
This cohort study highlights that low ALM is an independent predictor of executive function decline over 3 years in older community-dwelling populations. In this population, cognitive deficits can lead to severe consequences such as increased risk of falls, injuries, and even death. Maintaining a certain level of fitness to preserve and improve skeletal muscle mass is crucial. The findings presented in this study also proposed that routine assessment of muscle mass in the older population may help identify or stratify individuals at risk of cognitive decline. This may enable early interventions that mitigate the progression of sarcopenia-related cognitive impairments. Early screening in older individuals for sarcopenia and implementing non-pharmacological interventions, such as exercise, can be particularly helpful in delaying the progression of cognitive decline.
Regular physical activity, especially strength training along with aerobic exercise, has well-documented neuroprotective benefits, promoting brain health and function. Strength or resistance training is imperative to improve type 2 skeletal muscles, which are commonly atrophied in older individuals. However, a comprehensive exercise routine that incorporates strength training, aerobic activities, and functional/balance exercises is necessary for healthy muscle and brain aging. The contracting muscle triggers the release of key myokines. It communicates with the brain via the muscle-brain axis to promote anti-inflammatory and neuroprotective effects in the brain to enhance and maintain learning and memory. Although not addressed in this review article, proper nutrition and lifestyle are critical factors for maintaining muscle mass and cognitive function. Whether it may be for lifespan or healthspan purposes, it is even more critical as we age to maintain muscle mass through targeted exercises to support and preserve cognitive performance and overall health.
TAKE HOME POINTS
Sarcopenia is the process of muscle mass degeneration associated with aging. Loss of muscle mass is linked with impaired various domains of cognition, including memory, executive functions, and psychomotor speed.
The Canadian Longitudinal Study on Aging found that loss of ALM was an independent predictor of rapid decline in executive function over 3 years. Participants with lower ALM did have less physical activity/exercise at baseline compared to those who did not have lower levels of ALM.
Regular exercise in the older population is a non-pharmacological approach to prevent the progression of age-related cognitive impairments. Regular exercise has a wealth of health benefits, including neuroprotection and improved cognitive functions. Aerobic and resistance or strength training have proven beneficial for older adults. Aerobic exercise helps to preserve muscle mass while resistance training enhances muscle quality and strength.
The working skeletal muscles release important myokines such as BDNF, IL-6, and IGF-1, which have been shown to improve brain volume, learning, and memory. Increases in BDNF and IGF-1 in the hippocampus are correlated with improved learning and memory as well as increased hippocampal volume. On the other hand, IL-6 exhibits both pro- and anti-inflammatory actions, where elevated IL-6 results in inflammatory diseases. Aerobic and strength training reduce the level of IL-6, promoting anti-inflammatory effects.
Throughout aging, maintaining and improving brain health and function is critical through regular exercise. The World Health Organization recommends strength and functional training as well as aerobic exercise for older adults.
Citations
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.