Rapamycin
The most powerful tool to stop the acceleration of aging caused by mTOR dysfunction and cellular senescence.
The incidence of cancer increases exponentially as we age. One link between age-related cancer and degeneration could be an inflammatory tissue environment driven by MTOR in senescent cells. In her pivotal 2010 research paper, "The Senescence-Associated Secretory Phenotype: The Dark Side of Tumor Suppression," Dr. Judith Campisi delves into how senescent cells create to a cellular 'microenvironment' favorable for cancer progression. In this article, we review Campisi's important insights and explore the potential of rapamycin to mitigate the cancer-promoting tendencies of these dysfunctional senescent cells.
rapamycin
cancer prevention
17 mins
By: Daniel Tawfik
The incidence of cancer increases exponentially as we age. Unlike most age-related diseases, which generally cause cell and tissue degeneration and loss of function, cancer cells must acquire different, albeit aberrant, functions to progress to lethal disease. One link between age-related cancer and degeneration could be an inflammatory tissue environment driven by MTOR in senescent cells.
In her groundbreaking 2010 research perspective paper, The Senescence-Associated Secretory Phenotype: The Dark Side of Tumor Suppression, Dr. Judith Campisi from the Buck Institute for Research on Aging highlighted the tumor-promoting aspects of senescent cells. Campisi's research showcased the significant ability of senescent cells to reshape the cellular landscape around them, crafting what scientists term the 'microenvironment.'
Far from being an inert backdrop, this microenvironment serves as a dynamic stage upon which cells interact and potentially pave the way for disease progression, particularly cancer.
Central to Campisi's research is that while senescence can act as a defense against cancer, it may paradoxically promote it under certain conditions. Specifically, the pronounced release of pro-inflammatory molecules, the Senescence-Associated Secretory Phenotype (SASP), and its role in shaping a tumor-promoting environment are prominent highlights of her research.
In this article, we explore Campisi's research, delving deep into the role of the SASP, the intricacies of the microenvironment, and the overarching implications for tumor growth. We'll explore the impacts of senescent fibroblasts on breast and prostate cancer progression.
We delve into the intricate relationship between mTOR dysregulation and its influence on senescence as we age, examining how rapamycin might counteract the tumorigenic propensities of senescent cells. Throughout this exploration, a consistent theme surfaces: the paradoxical role of senescent cells in both protecting against and potentially fostering cancerous growth.
The concept of the tissue microenvironment is at the core of our understanding of cellular behavior and the pathology of cancer metastasis. It is, in essence, the neighborhood in which a cell resides, replete with its own set of rules and environmental factors.
The extracellular matrix (ECM) is central to this environment, a structural and functional web of proteins and carbohydrates that provides essential physical scaffolding for the cellular constituents and significantly influences cell behavior, migration, and function.
Much like a city teeming with activity and constant interactions, each tissue in our body is a bustling hub of cellular interactivity. These cells don't exist in isolation. They are surrounded by a milieu that includes other cells, molecules, physical factors, and the intricate network of the ECM. This dynamic network ensures that cells remain interconnected and in constant communication, dictating the overall health and function of tissues.
A chemical landscape is also at play in the cellular microenvironment. Local production of molecules like growth factors and cytokines adds another layer of complexity. Growth factors, for instance, might tell a cell to divide and multiply, while certain cytokines can call immune cells to an area, sounding an alarm of injury or infection.
These interactions are not just one-way. As cells respond to their environment, they also influence it, making the microenvironment a constantly evolving entity.
The significance of this intricate balance becomes evident when we consider the ramifications of its disruption. This disruption is what Campisi's research is attempting to explore. A classic example is cancer. Tumors, in particular, manipulate the microenvironment to their advantage, creating conditions conducive to their growth while sidelining healthy cells.
The relationship between a cancer cell and its surrounding environment is not a passive one. It's a dynamic and evolving partnership. The microenvironment has important effects on the ability of the cancer cell to evade the immune system and travel into adjacent tissues.
A key consequence of the disruption of the microenvironment is its impact on a cancer cell's capacity to evade the immune system. Under typical conditions, immune cells quickly identify and neutralize potential threats. Yet, cancer cells are adept at circumventing this defense, skillfully avoiding immune detection.
Campisi defines a "permissive microenvironment" as being like a cityscape transformed in such a way that it becomes a sanctuary for tumor cells. Within this modified setting, conditions are particularly conducive to the proliferation and heightened aggression of these cells.
By changing the composition of connective tissues surrounding them, these tumor cells can cloak themselves, evading the watchful eyes of the immune system. This not only lets them thrive locally but also gives them the chance to invade neighboring areas, a process analogous to metastasis or the spread of cancer to other parts of the body.
Campisi's research delves deep into the impact of senescent cells in cultivating such an environment. What characteristics of cellular senescence pave the way for these conditions?
Cells can be prompted into senescence by a myriad of factors. These could be extracellular cues, like harmful radiation or inflammatory molecules, or intracellular disturbances, like DNA damage. Essentially, when a cell senses that it's at risk or its internal machinery is compromised, it may decide to enter a state of permanent cell-cycle arrest.
At first glance, it might seem counterproductive for a cell to shut down. However, this is a strategic move. By halting their growth and division, senescent cells prevent any potential internal damage from being passed on to new generations of cells. This is especially crucial when considering the risk of replicating the cell into a fully formed tumor. In this context, senescence acts as a safety mechanism, ensuring that damaged or stressed cells don't evolve into cancerous entities.
All cells are exposed to growth stimuli. However, senescent cells respond differently to growth signals. Because senescent cells cannot divide when exposed to growth factors, they become hyperfunctional—they have a large morphology, are hyperactive, hyperinflammatory, and cause hyperplasia. While typical cells divide in response to growth stimuli, these stimuli intensify the detrimental hyper-functional behaviors of senescent cells [20].
Hyperplasia is a form of cellular proliferation that is characterized by an increase in the number of cells within an organ or tissue. Senescent cells excessively excrete mitogens, which stimulate cell replication of adjacent cells, which can be pathological, as in the case of cancer or benign tumors.
Hypertrophy, on the other hand, is an increase in the size of individual cells, leading to an overall increase in the size of the organ or tissue. However, if it persists for an extended period or becomes excessive, it can result in cellular dysfunction, tissue damage, or disease.
Hyperfunctionality refers to the increased activity of cells or organs beyond what is normal or necessary. Cellular hyperfunctionality can occur due to several factors, including excessive stimulation by hormones or growth factors or abnormal signaling pathways. Hyperfunctionality can result in cellular damage, dysfunction, or disease.
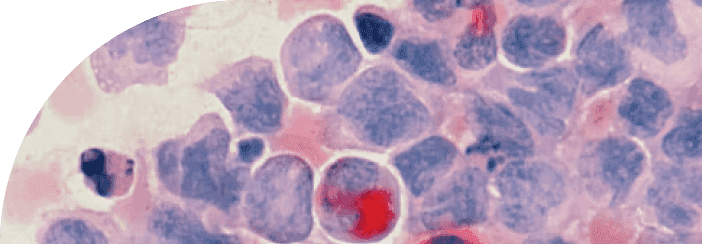
Across all cell types, one of the defining characteristics of a senescent cell is its excessive release of inflammatory molecules. Senescent cells release a "witch's brew" of pro-inflammatory cytokines, chemokines, growth and mitogenic factors, pro-senescent proteins, and proteases that make up the Senescent Associated Secretory Phenotype (SASP).
The SASP signals that a cell is under duress, effectively acting as an SOS signal to recruit immune cells to eliminate the damaged cell. As senescence progresses, the SASP overexpresses more of these inflammatory molecules, leading to chronic inflammation that drives tissue damage and degeneration over time. This altered secretory behavior over time of the SASP can inadvertently create conditions conducive to tumor growth.
The implications of the SASP for health, especially in relation to cancer, are profound. There is compelling evidence that numerous factors within the SASP can lay the groundwork for a cancer-friendly microenvironment [1]. Think of it as tilling the soil to favor the growth of a particularly aggressive weed.
Once the ground is prepared, it becomes conducive to the emergence and spread of this undesired invader. Similarly, the SASP aids not only in the initial formation of cancerous cells but also in their spread and aggression.
The tentacles of SASP-driven cancer spread far and wide. Research has connected it to tumors originating from an array of tissues: from the neurons in our brains [2], the ducts of our breasts [3], the layers of our skin [4], the lining of our stomach [5], the tissues in our mouth [6], the prostate gland [7], to the delicate tissues of the ovaries [8].
Diving deeper into the cellular level, a significant focus of scientific inquiry has been on senescent fibroblasts. One of the groundbreaking findings from Campisi's lab was that senescent fibroblasts can promote the growth of pre-cancerous and cancerous cells.
Fibroblasts are the workhorses of our body's connective tissues or stroma. They're numerous and play a pivotal role in crafting the structural foundation of our organs. Their responsibilities include:
Producing the framework of the stroma.
Laying down the basal membrane.
Releasing components of the extracellular matrix (ECM) as well as enzymes that can modify it.
Due to their long lifespan and their vital role in tissue architecture, it's understandable why they have been a prime subject of study [9].
Campisi found that the molecules secreted by senescent fibroblasts can stimulate nearby cells to proliferate and degrade or remodel the extracellular matrix, making it more conducive for tumor cells to invade and metastasize.
Other senescent cells, like the skin's keratinocytes [10], the cells lining our blood vessels [11], and even multipotent mesenchymal stem cells [12], have also been shown to create a permissive environment for tumorigenesis.
To truly grasp how the SASP can influence cancer development, one must dive into the intricate web of cellular signaling and regulation that governs it.
At the heart of this regulatory mechanism is the protein p53. Revered as the "guardian of the genome," p53 plays a crucial role in ensuring the stability of our genetic material. It's a key player in cellular responses to various stressors, especially DNA damage, and can decide the fate of a cell—whether it repairs, goes dormant (senesces), or self-destructs (undergoes apoptosis).
When we introduce cancer into the equation p53 activity can become dysfunctional and exacerbate the permissive microenvironment created by the SASP. In fact, the TP53 gene, responsible for producing p53, is commonly mutated in cancerous cells [13]. With a faulty TP53, the balance maintained by p53 could tip, leading to an exaggerated, unrestrained SASP response. The outcome? A persistent inflammatory environment within tumors, further fuelling their growth and aggression.
Cytokines IL-6 and IL-8, are particularly significant in their influence over the cancer development process. Cytokines, in essence, are protein molecules that play a crucial role in cell signaling, especially in immune responses. Within the expansive family of SASP molecules, IL-6 and IL-8 are overexpressed, making them pivotal players in the senescence landscape.
Researchers have delved deep into IL-6 and IL-8, unraveling a web of mechanisms through which they can boost tumor formation. One of the primary ways is by inducing the epithelial-to-mesenchymal transition (EMT) [14].
EMT is akin to giving epithelial cells, which are non-motile, a new identity, allowing them to act more like mesenchymal cells, which are more mobile and invasive. This enables them to break away from the primary tumor, invade the surrounding tissue, enter the bloodstream, and eventually form secondary tumors at distant sites.But the influence of IL-6 and IL-8 doesn't stop there. They also stimulate angiogenesis (the formation of new blood vessels), which provides growing tumors with the nutrients they require [14,15]. Moreover, they can disrupt the regular communication between cells [16], meddle with macrophage function (macrophages are essential cells in our immune response), and trigger broader innate immune responses.
In total, IL-6 and IL-8 are overexpressed in senescent cells and promote metastasis by:
Increasing the motility of cancerous epithelial cells to invade surrounding tissue.
Stimulate blood vessel formation, which gives the tumor access to nutrients they require to grow.
They help tumor cells evade the immune system.
The strongest evidence hails from xenograft studies, which involve transplanting cells or tissues from one species into another. In the realm of cancer research, xenografts often involve implanting human cancer cells into mice to study tumor progression.
In the Campisi study, senescent fibroblasts were co-injected into mice alongside either premalignant or cancerous epithelial cells. The presence of these senescent fibroblasts seemed to spur tumor formation and growth [17, 18, 19].
Delving deeper into the cause, researchers found that these senescent cells were producing VEGF (a factor that promotes the formation of blood vessels) and triggering angiogenesis [17], while also secreting a protein called MMP3 [19], known to degrade the extracellular matrix and facilitate tumor invasion.
The secreted MMP3 factors can foster a pro-tumorigenic environment. MMP3, as a part of the SASP, can influence neighboring cells, making them more susceptible to malignant transformation.
Campisi found that MMP3 would break down the structural components of the ECM, which can facilitate tumor cell invasion and metastasis. The disruption of the ECM not only allows cancer cells to move more freely but can also release growth factors sequestered in the matrix, further promoting cancer cell growth.
Like IL6 and IL8, MMPs can activate pro-angiogenic factors, leading to the formation of new blood vessels [17]. Tumors need blood supply to grow beyond a certain size, making angiogenesis a critical step in tumor progression.
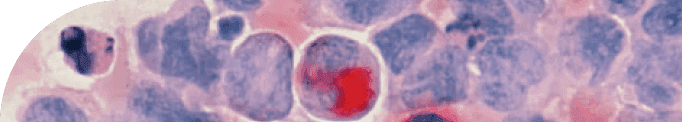
The development of breast cancer involves many different cell interactions within the breast tissue. Going back to Campisi's research, one of the main contributors to this complexity was senescent fibroblasts.
Campisi identified senescent fibroblasts as significant contributors to tumorigenesis in mammary glands. She found that the alteration in the tissue environment, influenced by the SASP, induced nearby epithelial cells to proliferate aberrantly.
Stromal cells are a diverse group of non-tumor cells that make up the supportive framework of tissues. In experiments in which stromal cells are irradiated or exposed to radiation, they are transformed to become senescent.
In these experiments, irradiated stromal cells change the mammary epithelial microenvironment, a region within the breast tissue composed of cells lining the milk ducts [17]. This disruption has promoted abnormal growth of these epithelial cells, which is a concerning factor for breast cancer development.
How did these senescent stromal cells lead to tumorigenesis?
As part of the transformation of the mammary gland microenvironment, matrix metalloproteinases (MMPs) play a role in degrading the extracellular matrix components to support the aggressive growth of cancer cells. Senescent fibroblasts secrete higher levels of MMPs [19].
Research suggests that these MMPs are a key factor behind the increased tumor-forming ability (or tumorigenicity) observed when breast epithelial cells are transplanted into mice. The reasoning is that MMPs, by degrading the extracellular matrix, can make it easier for growth-promoting and movement-inducing signals to reach and influence breast cancer cells [19].
Limiting cellular growth has been found to have positive outcomes for lifespan and healthspan. From worms to mammals, mutations that inactivate certain cell growth signaling pathways, such as the insulin/IGF-1 signaling pathway, have been shown to slow senescence and increase lifespan by up to sevenfold [20].
When we examine senescence, we find that the growth pathway at the core of its hyper-functions is the overactivation of the mTOR (Mammalian Target of Rapamycin) pathway. As such, targeting the mTOR pathway provides a promising approach to slow down or even reverse the effects of cellular senescence and age-related diseases.
mTOR is a complex that exists in every cell type and across all species. It serves as the air traffic control for determining when a cell should grow and divide and when it should not. mTOR turns on the cellular machinery to promote growth when nutrients, particularly amino acids (specifically leucine), are available, and it shuts down cellular growth when nutrients are scarce.
However, in senescent cells, mTOR activity is dysfunctional. In this dysfunctional state, mTOR amplifies its hypergrowth and functionality, resulting in excessive growth and overproduction of molecules of the SASP.
Additionally, it amplifies its resistance to apoptosis, making it difficult for these cells to undergo programmed cell death. This hyperactivation of MTOR is a major contributor to the dysfunction of senescent cells and the aging process.
From an evolutionary perspective, this makes a lot of sense—we would want to grow when there are ample nutrients to sustain growth, and when nutrients are low, mTOR stops cell growth and replication because of the lack of energy to do so.
When TOR is inhibited by the lack of sufficient nutrients, the cell will enter into a cleanup mode and use cellular debris within the cell as a fuel source. Any misfolded proteins or other toxic molecules will be consumed by the cell for energy. This cellular deep-cleaning process, in which a cell consumes its debris, is called autophagy.
Autophagy is an essential process for maintaining cellular health and preventing the accumulation of damaged or dysfunctional components. In addition to degrading and recycling cellular debris, autophagy can also provide nutrients to support cellular metabolism and maintain cellular energy levels.
When TOR is activated in a senescent cell, it amplifies the overexcretion of inflammatory molecules that are part of the SASP, leading to tissue damage and a permissive environment for tumor growth.
On the other hand, when autophagy is induced in senescent cells, the cell begins to degrade and recycle these toxic proteins, leading to a reduction in their production and less harm to the surrounding tissue.
In 2015, Campisi's lab did a follow-up study to study the role of mTOR in cellular senescence. The group explored the use of rapamycin to blunt the pro-tumorigenic phenotype of senescent cells.
To explore the role of mTOR in cellular senescence and the link between mTOR activity and the SASP, Campisi's lab exposed senescent human cells to rapamycin, which selectively inhibits mTOR complex 1 [21].
The study found that MTOR inhibition suppressed the secretion of inflammatory cytokines by senescent cells. Rapamycin reduced the secretion of ∼35% of the different SASP factors; importantly, it substantially decreased the secretion of the major SASP component IL-6 [21].
In cell culture, a single exposure of cells to rapamycin for only 24 h immediately after ionizing radiation suppressed IL6 secretion by ~80% for 7 days after that, similar to the suppression seen after continuous treatment for 7 days [21].
Lastly, when prostate tumor cells were grafted into mice together with senescent cells, tumor growth was enhanced, but the tumour-promoting effects of senescent cells were reduced if they were pretreated with rapamycin. This suggests that mTOR signaling promotes tumor growth in vivo.
As chemotherapy and radiotherapy induce cellular senescence, and such senescent cells might contribute to cancer relapse, the mTOR inhibitor rapamycin could potentially be used as adjuvant therapy for cancer. From these experiments, rapamycin seems to ameliorate age-related pathologies, including late-life cancer, by suppressing senescence-associated inflammation.
These findings from Campisi's lab underscore the potential of rapamycin as a therapeutic agent in combatting the harmful effects of senescent cells, especially in the context of cancer. The ability of rapamycin to mitigate the secretion of inflammatory molecules, even after a brief exposure, hints at its efficacy. The promising results in mouse models further bolster the case for its potential use in human applications. As we continue to decipher the multifaceted nature of cellular senescence and its implications, agents like rapamycin offer a beacon of hope in our ongoing battle against age-related diseases and cancer.
Citations
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.