Acarbose
Maximize Metabolism. Optimize Gut Health.
When the National Institute for Aging tested over a dozen longevity molecules, acarbose was one of five molecules shown to increase lifespan. The intrigue around acarbose stems from its dual function: it influences metabolic health and reshapes our gut microbiota. But how does this alteration in microbial balance translate to enhanced healthspan? This article probes the notion that the healthspan-promoting benefits of acarbose are intrinsically linked to its role in diversifying the gut microbiome and amplifying the production of short-chain fatty acids.
acarbose
nutrition
15 mins
By: Daniel Tawfik
Identifying effective anti-aging interventions that tangibly extend lifespan is a challenging endeavor. The process of aging is not governed by a single mechanism but by an intricate web of biological pathways. Further muddying the waters is the absence of long-term studies, unified definitions, and consistent methodologies for evaluating potential anti-aging solutions.
Recognizing this gap, the National Institute for Aging (NIA) has launched one of the most ambitious Interventional Testing Programs (ITP) to date. The aim? To rigorously test longevity drugs and shed light on the complex interplay of these biological pathways.
The ITP represents one of the foremost authorities in longevity research. Operating over an extended period, this program has meticulously analyzed various interventions that might enhance lifespan, utilizing a diverse genetic pool of mice and maintaining uniform protocols across its three distinct study locations.
A standout finding from this program is the pronounced impact of the drug acarbose on mouse longevity.
Acarbose is primarily known for its role in regulating blood sugar levels. By inhibiting enzymes like α-glucosidase and α-amylase, it effectively slows down the digestive breakdown of starch in the intestines, which subsequently reduces the spike in blood glucose levels following a meal.
Consistently, the ITP has shown that acarbose can significantly boost the median lifespan of the mouse model it was studying. This effect is particularly pronounced in male mice, where a remarkable 22% increase was noted when the treatment began at a young age of just 4 months [1].
In comparison, female mice displayed a more modest 5% boost in median lifespan under the same conditions [1]. Intriguingly, even when acarbose treatment was initiated later in life, at 16 months, a noticeable longevity benefit remained [2].
Beyond median lifespan, it's worth highlighting the 90th percentile lifespan metric, often considered a proxy for the maximum potential lifespan. Acarbose showcased its potency here as well, bestowing benefits of nearly equivalent magnitude in both male and female mice [1]. This suggests that the drug doesn't merely shift the average lifespan but might help more mice reach an older age than otherwise possible.
What accounts for these results?
Given acarbose's ability to lower post-prandial glucose levels, it's no surprise that acarbose has found its place in the therapeutic regimen for patients with type 2 diabetes [3]. Beyond its glycemic control capabilities, the drug showcases broader health implications, with studies demonstrating its potential to decrease the risk of cardiovascular diseases among the diabetic population [4].
However, when shifting the focus from diabetes to longevity, the mechanisms through which acarbose operates become less transparent.
It seems that acarbose's longevity-promoting impacts stem from more than just its ability to regulate blood sugar levels. The ITP examined the idea that these effects could be derived from its effects on the digestive system.
Why examine its effects on the digestive system?
By impeding the absorption of glucose from starch, acarbose redirects a more significant portion of polysaccharides, or complex carbohydrates, toward the lower digestive tract [5]. This action somewhat mirrors the benefits derived from fiber consumption, which is known to promote digestive health.
Concrete evidence supports this notion: studies have shown an uptick in starch content in the stool of those taking acarbose [5, 6]. Furthermore, an intriguing observation is the increased exhalation of hydrogen in breath tests [7–11], suggesting that the undigested starch reaching the colon is actively being fermented by our resident gut bacteria, or microbiota.
Acarbose's effects on the gut microbiota and the resulting production of short-chain fatty acids (SCFAs) during fermentation have been a focal point of scientific intrigue. However, there's a significant gap in our knowledge: while theoretical frameworks and findings from various animal models hint at a link between acarbose, gut microbiota, and enhanced longevity, no study, until recently, has directly investigated this potential connection in mice.
Stepping into this research void, the ITP, headed by Dr. Rich Miller, embarked on an ambitious study to probe deeper into this hypothesis. Their exploration was hinged on four key predictions:
Acarbose consistently alters the bacterial community structure within the gut.
Mice treated with acarbose exhibit elevated concentrations of SCFAs.
There's a discernible correlation between the gut microbial community structure and the presence of SCFAs and other metabolites, irrespective of whether the mice are on acarbose or not.
And perhaps most intriguingly, the concentrations of SCFAs could potentially serve as predictors of lifespan.
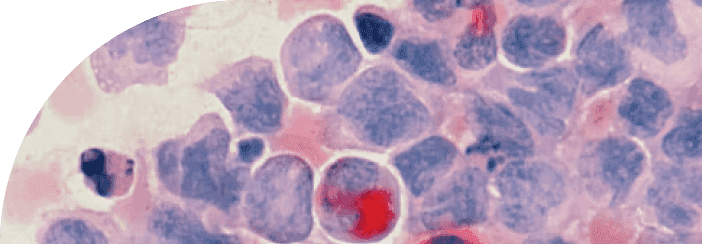
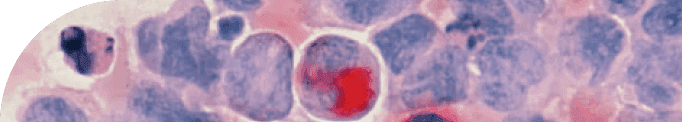
To explore the overall hypothesis that changes to the gut microbiome and the secondary effects on the increase in SCFA's, the ITP compared the fecal microbiome of mice treated with acarbose to control mice.
To ensure comprehensive and replicable results, fecal samples were meticulously analyzed from both control and acarbose-treated mice. This rigorous analysis wasn't restricted to just one location; samples were sourced from mice enrolled in the ITP protocol across three distinct, independent study sites, reinforcing the breadth and depth of the research.
Acarbose's influence on the microbial residents of the gut emerged as a central theme in the study, with evidence revealing distinct variations in the gut bacterial communities of acarbose-treated mice compared to control groups across all three study locations. These results substantiate the idea that acarbose seems to be remodeling the gut microbiome.
Miller's study showed consistent increases in SCFAs, particularly acetate, and butyrate, were consistently observed in different samples, such as human fecal matter, blood serum, and rodent portal blood and cecal contents.
The elevation in SCFA production was linked to changes in the gut microbial community. For instance, the growth of specific bacterial families was associated with increased SCFA production.
Key bacterial families such as Muribaculaceae, Lachnospiraceae, and Lactobacillaceae show specific correlations with certain SCFAs. For instance, Muribaculaceae shows a strong correlation with propionate, a short-chain fatty acid with various health implications.
The correlations were consistent across different study sites, hinting that they weren't just due to localized factors at each research location. This consistency across sites adds strength to the findings, suggesting that the observed microbial-SCFA relationships are more universal than situational.
Across all three sites, acarbose increased the median male survival of the underlying study population by 17% from 830 to 975 days.
Male vs. Female Longevity Impact: Acarbose's effect on male longevity is notably significant. The increase of 17% in median male survival, which translates to an additional 145 days (from 830 to 975 days), is substantial. This means that, on average, male subjects lived almost five months longer when treated with ACA. For females, there was also an increase in longevity, but it was more modest at 5%, or an extra 42 days (from 889 to 931 days).
The statistical results (log-rank test P<0.001 for males and P=0.003 for females) strongly suggest that these observed increases in longevity are not due to random chance. Instead, they are likely a genuine effect of acarbose on the study population. The log-rank test is a common method used to compare survival times between two groups, so its use here adds credibility to the results.
The ITP appears to substantiate the hypothesis that the longevity benefits of acarbose in the mouse model related to changes in the activity of microbial communities in the gut associated with the increased influx of starch, and possibly attributable to known health effects of microbial metabolites, including SCFAs.
Not only were changes observed in the microbial composition of the gut, but there was also a notable alteration in the products of fermentation, pointing directly to the influence of acarbose. Most interestingly, a correlation was found between fecal SCFA concentrations and longevity in the mice. Simply put, higher SCFA concentrations seemed to imply a longer life.
But what are the mechanisms by which SCFAs contribute to longer healthspan?
SCFAs are vital to gut health and overall well-being. The primary members of this group, namely acetate, butyrate, and propionate, serve diverse functions, ranging from energy sources for the body to modulators of inflammation and other gut functions.
Each of these SCFAs has its own set of physiological roles in the body, from energy provision to gut health and immune modulation. By affecting all of them, acarbose could potentially impact a myriad of metabolic and physiological processes [12].
SCFAs, particularly butyrate and acetate, have been shown to possess anti-obesity properties in rodents [13]. When mice were given diets enriched with these SCFAs, they displayed increased energy burning, thereby resisting obesity. Such findings underscore the potential of SCFAs in influencing body weight [14].
Acetate and propionate seem to have notable effects on regulating blood sugar levels. Propionate in particular, when administered to humans in the form of an inulin-propionate ester, appeared to regulate hunger hormones (GLP-1 and PYY) leading to reduced calorie consumption and less weight gain over time [15]. The link between SCFAs, hunger-regulating hormones, and glucose homeostasis is important.
Histone acetylation is akin to a cellular switch, toggling between promoting gene transcription (through acetylation) and suppressing it (via deacetylation). It majorly occurs on histones 3 and 4 and is controlled by two types of enzymes: histone acetyltransferases (HATs) which add acetyl groups, and histone deacetylases (HDACs) which remove them.
HDACs, in particular, are under the spotlight because of their role in cancer therapy and anti-inflammatory responses. Intriguingly, SCFAs, specifically butyrate and propionate, have emerged as natural HDAC inhibitors [16].
Among SCFAs, butyrate is the star molecule. Present in high concentrations in the gut, it serves dual functions: it's a primary energy source for colon cells and acts as a protective agent against colorectal cancer and inflammation. Herein lies the butyrate paradox. In healthy colon cells, butyrate is primarily an energy substrate promoting growth, whereas, in cancer cells, it suppresses growth by acting as an HDAC inhibitor [17].
A potential explanation for this dichotomy is the metabolic preferences of the cells. Healthy colon cells predominantly utilize butyrate for energy, whereas cancer cells favor glucose. Butyrate accumulates in greater concentrations in cancer cells, becoming an efficient HDAC inhibitor. Thus, while butyrate might activate HATs in normal cells, it inhibits HDACs in cancerous ones. The nuances of this mechanism, such as the protection of stem cells in the colon from high butyrate concentrations, further underscore its complexity and context-specific impact.
Butyrate's influence doesn't stop with cancer. As an HDAC inhibitor, it also suppresses pro-inflammatory agents, fine-tuning our immune system to respond judiciously. Butyrate's interaction with immune cells, from macrophages to T cells, plays pivotal roles in immune homeostasis [18].
SCFAs, in general, regulate cytokine expression in T cells and aid in the generation of regulatory T cells (Tregs) — vital for immune system balance. The metabolic shifts in activated T cells make them receptive to SCFA-mediated HDAC inhibition, resulting in enhanced immune modulation [19].
Interestingly, acetate, previously not considered an HDAC inhibitor, has been found to exhibit inhibitory actions on HDACs in activated T cells. This highlights that the entire family of SCFAs could be potential modulators of our health, not just the more commonly studied molecules like butyrate [19].
In a nutshell, SCFAs, with their HDAC-inhibiting properties, are promising candidates for a range of health benefits. From acting against tumors to modulating the immune response, they exemplify the deep interconnection between our gut environment and overall health. As we delve deeper into understanding SCFAs' roles, the intricate dance of molecules in our gut is set to rewrite the rules of health and disease.
Only about 10% of all cancers arise from inherited genetic mutations. This means that a vast majority have roots in acquired somatic mutations and environmental influencers. A surprising revelation in this context is the role of gut microbiota. Recent studies suggest that up to 20% of all global cancer cases are somehow connected with microbial infection [20].
Chronic inflammation, especially in the colorectal region, significantly elevates the risk of developing colorectal cancer (CRC) [21]. Interestingly, not just pathogenic but even some of our friendly gut bacteria have been linked with this inflammation and subsequent cancer development. This makes the role of commensal bacteria in our gut ambiguous, as they can both trigger and suppress inflammation and cancer, contingent upon various factors.
Antibiotics, which disrupt our microbiota, can prevent chronic colitis, suggesting that some of our gut's normal residents have a pro-inflammatory role. However, when deprived of their usual microbiota either through a germ-free environment or antibiotics, mice become more susceptible to certain inflammation triggers, hinting at the multifaceted roles of these microorganisms [22].
Delving deeper, we find that some microbial metabolites, like SCFAs, act as defenders against inflammation. Their presence is not just an indicator of a healthy microbiome but also plays a pivotal role in maintaining the gut's integrity and regulating the immune response. Activation of a specific receptor, Free Fatty Acid Receptor 2 (FFAR2), by one such SCFA (acetate) provides marked protection against inflammation in mice. FFAR2 activation can suppress inflammation, which is beneficial in inflammatory disorders like inflammatory bowel disease (IBD) and asthma. FFAR2 is expressed in various immune cells, including neutrophils, monocytes, and eosinophils. Given its role in inflammation, energy metabolism, and immune cell function, FFAR2 presents a promising therapeutic target for various diseases, including metabolic disorders, inflammatory diseases, and certain cancers.
This brings into focus SCFA receptors like GPR109A and FFAR2, whose expression levels dramatically reduce in colon cancer cases. This drop reinforces the protective aspect of SCFA signaling, with butyrate standing out as a potential key player. Evidence points towards butyrate's protective influence, given the observed decline in butyrate-producing bacteria in ulcerative colitis and colon cancer patients and its potential protective effects against experimental colitis [22].
SCFAs also interact with our brain. Intriguingly, acetate, another SCFA, when administered intravenously, can cross the protective blood-brain barrier, activating neurons that signal satiety. More profound is the relationship between SCFAs and microglia—the sentinels of our brain and spinal cord. Germ-free mice, devoid of their regular microbial companions, exhibit a distinct microglia pattern in their brains. Introducing SCFAs restores the balance, emphasizing the importance of SCFAs in neuro-immunity [23].
Furthermore, SCFAs play a pivotal role in regulating the blood-brain barrier's integrity. Notably, certain microbial allies, known for their SCFA-producing prowess, alongside direct butyrate exposure, enhance the barrier's permeability. This action is associated with promoting the growth of new blood vessels and nerve cells, accentuating the protective role SCFAs play in our brain's sanctum [24].
Inflammation is a hallmark of aging. As individuals grow older, their bodies produce higher levels of pro-inflammatory factors compared to the younger population. This upsurge is often indicative of aging and is linked with age-related diseases. Studies using model organisms like C. elegans reveal how integral pathways, such as the TGF-β, p38 mitogen-activated protein kinases, and the DAF-2 insulin pathway, regulate innate immune functions [25].
Disruptions in these pathways can lead to increased inflammation and impact longevity. For instance, centenarians, individuals who live to or beyond 100 years, have notably lower levels of interleukin (IL)-6, a pro-inflammatory factor. This observation is intertwined with a balanced intestinal environment, indicative of a robust immune function [25].
With age, the diversity of our gut microbiota dwindles, leading to an imbalance known as dysbiosis. This dysbiosis can trigger low-grade inflammation, disturbing the gut's environment, culminating in epithelial dysfunction. Consequently, the host becomes more susceptible to infections and unhealthy aging patterns. Several studies point towards a link between the gut microbiota's state, inflammation, and lifespan [25].
Intestinal alkaline phosphatase (IAP), an enzyme with anti-inflammatory properties, plays a pivotal role in mitigating bacteria-driven pro-inflammatory agents. In studies, mice devoid of IAP exhibited premature aging due to inflammation. In contrast, IAP supplementation helped maintain a balanced gut environment, staved off inflammation, and increased lifespan [25].
Similarly, dietary interventions, like inulin, have shown promise. Inulin enhances the levels of beneficial bacteria, such as Lactobacillus, which subsequently suppresses the expression of inflammatory genes.
Probiotics, like Probiotic-4, which comprises strains like Bifidobacterium lactis and Lactobacillus acidophilus, have been observed to decrease IL-6 levels, a cytokine negatively correlated with longevity [25].
The downstream effects of inflammation reduction have significant implications for longevity. For example:
Increased inflammatory activity has been linked to brain aging, but acarbose, a medication that inhibits the activation of the hypothalamic nuclear factor kappa B (NF-κB) inflammatory pathway, has been shown to delay aging in mice. Acarbose has been found to inhibit the activation of interferon-γ inducible protein-10, monocyte chemoattractant protein-1, macrophage-derived chemokine, and TNF-α, and to downregulate NF-κB-P65 activity in human monocytic THP-1 cells.
Furthermore, the levels of IL-6 in patients with diabetes treated with acarbose are also significantly reduced.
Adipose tissue is a significant source of inflammation. There is evidence that acarbose has the ability to curb adipose tissue inflammation.
Acarbose reduces the expression levels of inflammatory factors by increasing the abundance of beneficial bacteria. Many species of these anti-inflammatory bacteria are recognized as short-chain fatty acid-producing bacteria that exert anti-inflammatory effects. These findings provide strong evidence for the anti-inflammatory potential of acarbose.
TAKE HOME POINTS
Acarbose emerges as a compelling agent in the pursuit of increased healthspan and longevity. By actively remodeling the gut microbiome, this drug serves as a bridge between our gut health and overall vitality. Its role in ensuring more starch reaches the colon nurtures a thriving environment for beneficial bacteria, particularly those that produce short-chain fatty acids (SCFAs). The consequential surge in SCFAs not only underscores anti-inflammatory effects but also supports overall metabolic health.
Furthermore, the ability of acarbose to reduce inflammatory markers, especially in the complex backdrop of age-related diseases, offers a glimpse into its potential. By inhibiting specific inflammatory pathways and boosting beneficial bacteria like Ruminococcus and Bifidobacterium, which are renowned for their anti-inflammatory properties, acarbose is more than just an anti-hyperglycemic agent. It stands as a beacon for how pharmaceutical interventions can potentially extend the health and longevity of individuals by targeting gut health.
In essence, acarbose exemplifies the future of targeted interventions – where longevity is not a mere byproduct but a conscious outcome steered by understanding and nurturing our gut's ecosystem.
Citations
.
14.
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.