Heart Vitality Panel
The Heart Vitality Panel goes beyond traditional lipid tests, it provides a comprehensive view of heart health risks, empowering proactive care with precision.
In this research narrative review, we explore the relationship between cholesterol, cardiovascular health, and longevity, emphasizing the multifaceted role of cholesterol beyond its conventional association with cardiovascular diseases. We discuss the significant roles of triglycerides and HDL in cardiovascular and metabolic health, emphasizing the triglyceride-to-HDL ratio as a critical indicator of metabolic dysfunction and cardiovascular risk. We emphasize the mechanisms by which these lipids influence carbohydrate metabolism and cholesterol flux, and the importance of managing elevated triglycerides through lifestyle interventions. Additionally, the article highlights the correlation between optimal metabolic health and enhanced cardiovascular function in athletes, demonstrating how metabolic efficiency supports heart health. By advocating for a comprehensive approach to lipid management that encompasses broader health assessments, we aim to refine strategies for cardiovascular disease prevention and treatment.
Lab Testing
Biomarkers
Exercise
Lipids
Cardiovascular Health
14 mins
By: Dr. Richard Cohen, Shriya Bakhshi
When discussing heart health, cholesterol is frequently emphasized as a key factor. However, the conversation about heart health and cholesterol involves greater complexities than might initially seem apparent. Although cholesterol is widely recognized for its association with cardiovascular disease risks, such as heart attacks and strokes, its role in the body is both complex and multifaceted. It affects not only cardiovascular health but also various other vital physiological functions.
Dr. Rick Cohen, a distinguished physician specializing in longevity medicine with over 20 years of experience and the current leader of the Healthspan Medical Advisory Board, has extensively explored these complexities. As the chief architect of Healthspan’s new advanced lipid panel, Dr. Cohen brings a deep understanding of the multifunctional roles of cholesterol. His insights underscore the importance of a nuanced approach to assessing cardiovascular health that extends beyond traditional markers.
In this article, we delve into the nuanced discussions held with Dr. Cohen regarding cholesterol's role in longevity. We will explore its dual nature—not only as a potential risk factor for cardiovascular diseases but also as an essential component for cellular integrity and function. Additionally, we will discuss the comprehensive methods and metrics employed by the advanced lipid panel designed under his guidance, emphasizing that a thorough assessment encompasses far more than cholesterol levels alone. This holistic approach allows for a deeper understanding of cardiovascular wellness within the broader context of overall health, paving the way for more effective management and optimization strategies.
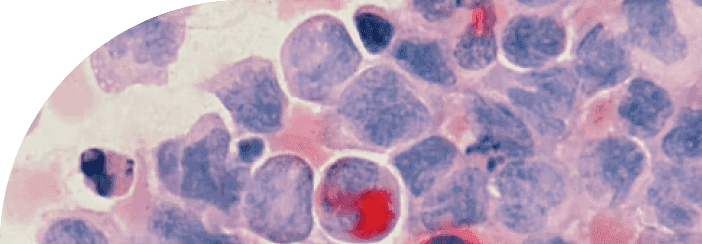
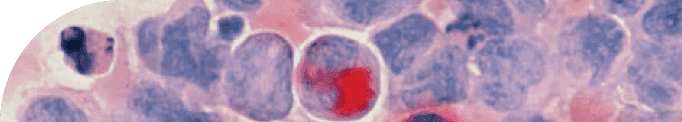
Cholesterol is a type of lipid, which is a category of fat-like substances that are essential components of cells and sources of energy. Lipids are crucial for various bodily functions, including forming cell membranes, acting as signaling molecules, and serving as a storage form of energy. Cholesterol, specifically, is vital for building and maintaining cellular structures, producing hormones, and aiding in digestion.
In the context of blood transport, cholesterol doesn't travel freely; it's carried by lipoproteins, which are complexes made of lipids and proteins. These lipoproteins act as transport vehicles in the bloodstream, carrying cholesterol to different parts of the body where it's needed. The two main types of lipoproteins involved in cholesterol transport are Low-Density Lipoprotein (LDL) and High-Density Lipoprotein (HDL).
Low-Density Lipoprotein (LDL) carries cholesterol from the liver, where it's produced, to various tissues and organs. Carrying cholesterol to organs is vital because it supplies the necessary components for cell membrane structure and hormone synthesis, essential for proper bodily function. While LDL is an essential component, persistently high levels of it can lead to a buildup of cholesterol in the arteries, which can form plaque and increase the risk of heart disease and stroke.
High-Density Lipoprotein (HDL) works in the opposite direction, carrying cholesterol away from the arteries and back to the liver, where it's either broken down or expelled from the body. This process is essential because it helps prevent the accumulation of cholesterol in the arteries, reducing the risk of plaque formation and cardiovascular diseases.
Understanding the roles of LDL and HDL in cholesterol transport helps clarify why managing the balance between these two types of lipoproteins is crucial for maintaining cardiovascular health.
The significance of cholesterol in the body extends beyond its association with heart health. Cholesterol is a fundamental component necessary for various bodily functions. It ensures cell membranes maintain both structural integrity and the right level of fluidity, allowing cells to operate effectively and interact with their surroundings.
Furthermore, cholesterol serves as a building block in the synthesis of vital steroid hormones, such as testosterone and estrogen, and adrenal hormones that are key regulators of metabolism, immune response, and the body's stress management. Additionally, it plays a crucial role in the skin's production of vitamin D when exposed to sunlight, a process essential for bone health and robust immune function.
Cholesterol also facilitates the production of bile acids in the liver, which are indispensable for the digestion and absorption of dietary fats. This underscores the complexity and necessity of cholesterol in supporting and maintaining the body's overall health and well-being.
Our understanding of cholesterol's role in heart health has evolved significantly over the years. Initially, cholesterol was seen as the main villain in heart disease, leading to widespread campaigns to reduce its levels in the body. However, it became apparent that the relationship between cholesterol and heart health is more complex than previously thought. Cholesterol, particularly when viewed through the lens of lipoprotein particles like LDL (low-density lipoprotein) and HDL (high-density lipoprotein), plays a nuanced role in the cardiovascular system. LDL is no longer universally labeled as "bad," nor is HDL simply "good." The impact of these lipoproteins on heart health depends on various factors, including particle size, density, and individual biochemical variability [1].
This shift in understanding emphasizes the importance of looking beyond just cholesterol levels to assess cardiovascular risk. Factors such as metabolic health, inflammation, and the individual's genetic and lifestyle context have gained attention for their roles in heart disease. For instance, the interaction of cholesterol with other elements like inflammatory markers, blood sugar levels, and blood pressure provides a more comprehensive view of cardiovascular health. This holistic approach recognizes that heart health cannot be distilled to a single metric like cholesterol levels but instead must be assessed within the broader context of overall bodily health and individual patient differences.
Triglycerides play a vital role in metabolism as the main form of stored energy in the body, yet they are often overshadowed by other lipids in traditional medical assessments. When excess carbohydrates are consumed, they are converted into triglycerides and either stored in fat cells or remain circulating in the bloodstream. Elevated triglyceride levels, commonly observed in individuals who consume more carbohydrates than their bodies can efficiently process, highlight the importance of carbohydrate management [2].
The ratio of triglycerides to HDL cholesterol is particularly crucial for assessing metabolic health, with an ideal ratio being close to 1:1. An imbalance in this ratio can indicate poor carbohydrate metabolism and potential metabolic dysfunction, increasing the risk of cardiovascular disease and diabetes.
Historically, triglycerides have not been the primary focus in Western medicine, partly because direct interventions aimed at reducing triglyceride levels did not consistently demonstrate a reduction in heart disease risk. However, it is increasingly recognized that high triglyceride levels should be viewed as indicators of broader metabolic issues rather than isolated factors.
Effective management of elevated triglycerides involves addressing their root causes through lifestyle changes. These changes include dietary modifications to reduce excessive carbohydrate intake, increasing physical activity, and enhancing insulin sensitivity. Such interventions adopt a holistic approach, focusing on preventing and treating underlying metabolic disturbances rather than merely targeting individual symptoms [2].
Furthermore, recent shifts in cardiovascular health research have led to a reevaluation of the role of HDL cholesterol, traditionally known as the "good" cholesterol. Although high levels of HDL cholesterol are generally viewed as beneficial, they do not always protect against cardiovascular disease. The functionality of HDL, especially its role in removing oxidized lipids from cells and promoting cholesterol flux, is now considered a more critical indicator of cardiovascular health. Cholesterol flux refers to the dynamic process by which cholesterol is transported away from arterial walls, an essential function in preventing atherosclerosis [2].
Understanding the relationship between triglycerides, HDL cholesterol, and metabolic health is crucial for effectively managing and improving cardiovascular outcomes. By emphasizing the significance of the triglyceride-to-HDL ratio and addressing lifestyle factors, healthcare providers can more accurately predict and mitigate risks associated with cardiovascular diseases. Additionally, the evolving perspective on HDL functionality highlights the importance of focusing on the dynamic processes of lipid management in cardiovascular health, rather than solely on static levels. This integrated approach aligns with a more holistic view of health, emphasizing prevention and the management of underlying metabolic conditions.
Optimal metabolic health significantly influences cardiovascular health, as is particularly evident in athletes, who exemplify peak metabolic and cardiovascular function. They maintain efficient mitochondrial function, crucial for energy production and reducing reactive oxygen species—byproducts that contribute to oxidative stress and inflammation, both linked to cardiovascular disease. Well-functioning mitochondria ensure the body's energy needs are met effectively, supporting overall heart health [3].
To understand this concept better, let’s think about a professional cyclist. The high physical activity levels typical of professional cyclists improve the body’s ability to manage glucose and insulin levels, reducing the risk of insulin resistance—a condition associated with increased inflammation and heart disease risk. Regular intense exercise helps maintain insulin sensitivity, ensuring glucose levels are appropriately managed and reducing cardiovascular stress.
Athletes like professional cyclists also benefit from improved blood viscosity and vascular health. Their physically conditioned bodies ensure that their blood is less viscous, which facilitates smoother blood flow and reduces strain on the heart. Moreover, regular high-intensity exercise contributes to more flexible and resilient arterial walls, reducing the likelihood of arterial stiffness, a factor in hypertension and cardiovascular complications.
An athlete’s heart is typically more efficient at pumping blood and supplying oxygen to tissues, critical during high-intensity performances. This efficiency also translates to a superior ability to handle physical stressors, evident in the rapid heart rate recovery after intense exercise. The speed at which an athlete’s heart rate returns to baseline after peaking during physical exertion is a strong indicator of cardiovascular fitness and resilience.
Finally, the true testament to an athlete's cardiovascular health is their ability to recover quickly from intense activity. This rapid recovery indicates a robust autonomic nervous system, reducing the likelihood of cardiovascular issues that can occur with poor recovery post-exercise.
The connection between metabolic health and heart health in athletes, particularly those engaged in cardiovascular-intensive sports like cycling, illustrates how efficiently the body can handle internal biochemical processes and external physical demands. This relationship underscores the importance of regular, balanced physical activity as part of a strategy to maintain optimal cardiovascular health [3].
In the realm of cardiovascular health, understanding the roles of specific lipids like lipoprotein A (Lp(a)) and apolipoprotein B (ApoB) is crucial in assessing risk and determining treatment strategies. Lp(a) is a lipoprotein particle similar to LDL cholesterol but includes a protein called apolipoprotein(a), which can contribute to the buildup of plaques in arteries, leading to atherosclerosis if levels are elevated. ApoB is a primary protein found in LDL and VLDL particles and is a marker of the total number of atherogenic particles in the bloodstream, making it a strong indicator of cardiovascular disease risk. [4]
Emerging insights suggest that a more nuanced approach may be necessary, emphasizing individual risk assessment, the cost-benefit analysis of lipid-lowering treatments, the crucial role of metabolic health, and the broader health implications beyond mere lipid levels.
Cardiovascular disease manifests uniquely in each individual, challenging the one-size-fits-all approach to lipid management. Traditional markers such as Lp(a) and ApoB are known contributors to arterial damage and heart disease. Yet, their presence alone does not universally predict cardiovascular events. Some individuals with high levels of these lipoproteins maintain excellent arterial health and flexibility, while others with lower levels may still experience significant cardiovascular problems. This variability underscores the necessity of personalized cardiovascular care that goes beyond standard lipid profiles to incorporate a comprehensive evaluation of each person's unique physiological landscape, including genetic factors, lifestyle, and other health conditions. [4]
Additionally, the decision to lower lipid levels, particularly through pharmaceutical interventions, involves significant considerations both in terms of costs and potential side effects. While statins and other lipid-lowering medications are standard treatments, they are not without risks and financial burdens. For some individuals, the benefits of marginally lower lipid levels may not justify the expense and potential for adverse effects. This aspect of cardiovascular care requires healthcare providers to carefully weigh the expected benefits of lipid-lowering against the drawbacks, ensuring that treatment decisions are economically sensible and aligned with the patient's overall health goals and conditions. [5]
The influence of metabolic health on cardiovascular risk is also profound and often underappreciated. Efficient glucose management, a healthy diet, and avoidance of harmful fats significantly impact vascular health and the body's overall inflammatory state. Metabolically healthy individuals—those who manage their glucose levels well and avoid dietary pitfalls such as excessive oxidized omega-6 oils—are less likely to experience the damaging effects of high lipoproteins. This fact points to the importance of addressing metabolic health as a primary strategy for preventing cardiovascular disease. By focusing on improving metabolic health, clinicians can impact a broad range of factors that contribute to cardiovascular health, potentially reducing the need for aggressive lipid-lowering strategies.
Focusing solely on lipid levels may overlook more critical factors that contribute to cardiovascular health. Lipids are often considered mere bystanders in the complex process of cardiovascular disease, which is more significantly influenced by systemic inflammation, immune system function, and metabolic disorders. For instance, an individual with optimal lipid levels but poor metabolic health remains at risk for various health issues, including cardiovascular events. This broader perspective necessitates a holistic approach to cardiovascular health, one that considers how interconnected physiological processes and lifestyle choices contribute to overall health and disease risk.
Assessing heart health is a nuanced process that extends far beyond the simple measurement of lipid levels. While lipids are undoubtedly important, they represent just one component of a multifaceted puzzle. To thoroughly evaluate heart health, a comprehensive approach that considers various factors and utilizes multiple diagnostic tools is essential to fully understand an individual's cardiovascular risk.
Several key indicators characterize a healthy heart. Efficient pumping capability is fundamental, as the heart must effectively circulate blood throughout the body to meet physiological demands without excessive strain. Optimal blood pressure is also crucial, as chronic high blood pressure can cause significant damage to the heart and arteries, heightening the risk of heart disease. Moreover, maintaining healthy arteries that are flexible and free from significant plaque buildup ensures they can adequately accommodate blood flow and adapt to changes in pressure and volume. While balanced lipid levels are just part of the equation, maintaining appropriate levels of cholesterol and triglycerides is vital to prevent the development of atherosclerotic plaques. [6]
To achieve a comprehensive assessment of heart health, several diagnostic tests can be utilized:
Blood Tests: These tests are crucial for measuring lipid profiles, including HDL, LDL, and triglycerides. They also evaluate inflammatory markers such as C-reactive protein (CRP) and other indicators like homocysteine that can provide insights into heart health.
Electrocardiogram (ECG): An ECG records the electrical activity of the heart, aiding in the detection of irregular heart rates, rhythms, and potential muscle damage.
Echocardiogram: This ultrasound-based test produces detailed images of the heart's structure and function, assessing aspects like valve operations and chamber sizes.
Stress Tests: By monitoring the heart's performance during physical exertion, these tests gauge how well the heart handles activity and its recovery rate, offering valuable information about cardiovascular resilience.
Coronary Calcium Scan: This imaging test identifies calcified plaque within the arteries, serving as an early indicator of atherosclerosis and an increased risk for heart disease.
Carotid Ultrasound: Focused on the carotid arteries in the neck, this ultrasound assesses plaque accumulation and evaluates stroke risk.
Integrating lipid measurements with other health indicators and considering lifestyle factors are crucial for a thorough evaluation and management of cardiovascular risk. This comprehensive approach enables more accurate and personalized strategies to promote heart health and prevent cardiovascular disease, ensuring a broader understanding and better management of an individual's overall heart health.
Cholesterol is not just a solitary marker of cardiovascular risk but a pivotal substance essential for numerous biological functions, from cellular structure integrity to hormone production. Our evolving understanding of cholesterol, particularly its transport via lipoproteins like LDL and HDL, highlights the intricacies of its roles and the complexities of managing heart health. While traditional views have simplified cholesterol into "good" and "bad" categories, modern research advocates for a more nuanced approach, considering individual metabolic health, lifestyle factors, and genetic predispositions.
This refined perspective emphasizes the importance of holistic cardiovascular care that goes beyond cholesterol levels to include a wide array of metabolic and physiological factors. By integrating this knowledge with lifestyle modifications and targeted therapies, we can more effectively address the multifaceted nature of cardiovascular health. The journey towards heart health is not solely about managing lipids but understanding and optimizing the interplay between all contributing factors, ensuring a comprehensive approach to prevention and treatment of heart disease.
TAKE HOME POINTS
Complex Role of Cholesterol: Cholesterol's impact on health extends beyond the traditional focus on cardiovascular disease. Cholesterol is crucial for cellular structure, hormone production, and digestion, influencing a range of physiological processes.
Reevaluation of Lipoproteins (LDL and HDL): Factors such as metabolic health, inflammation, and the individual's genetic and lifestyle context have gained attention for their roles in heart disease. For instance, the interaction of cholesterol with other elements like inflammatory markers, blood sugar levels, and blood pressure provides a more comprehensive view of cardiovascular health.
The Importance of Ratio of Triglycerides to HDL to Measure Metabolic Health.The ratio of triglycerides to HDL cholesterol is particularly crucial for assessing metabolic health, with an ideal ratio being close to 1:1. An imbalance in this ratio can indicate poor carbohydrate metabolism and potential metabolic dysfunction, increasing the risk of cardiovascular disease and diabetes.
HDL's Role in Promoting Cholesterol Flux: The functionality of HDL, especially its role in removing oxidized lipids from cells and promoting cholesterol flux, is now considered a more critical indicator of cardiovascular health. Cholesterol flux refers to the dynamic process by which cholesterol is transported away from arterial walls, an essential function in preventing atherosclerosis.
Signatures of Peak Metabolic Health in Athletes: Optimal metabolic health significantly influences cardiovascular health, as is particularly evident in athletes, who exemplify peak metabolic and cardiovascular function. They maintain efficient mitochondrial function, crucial for energy production and reducing reactive oxygen species—byproducts that contribute to oxidative stress and inflammation, both linked to cardiovascular disease.
Athletes and Vascular Health: Athletes like professional cyclists also benefit from improved blood viscosity and vascular health. Their physically conditioned bodies ensure that their blood is less viscous, which facilitates smoother blood flow and reduces strain on the heart.
The Role of Lp(a) and ApoB in Cardiovascular Risk Assessment: In cardiovascular health, the roles of lipoproteins such as Lp(a) and ApoB are essential for risk assessment and treatment strategies. Lp(a) is a lipoprotein similar to LDL but includes apolipoprotein(a), which can lead to plaque buildup and atherosclerosis when elevated. ApoB is found in LDL and VLDL particles, serving as a marker for the total atherogenic particles in the blood, thus indicating cardiovascular disease risk.
More Nuanced Analysis is Required: While traditional lipid markers like Lp(a) and ApoB are linked to arterial damage and heart disease, they do not consistently predict cardiovascular events due to individual differences in arterial health and other factors.
The Importance of Metabolic Health on Cardiovascular Risk. The impact of metabolic health on cardiovascular risk is significant yet often overlooked. Proper glucose management, a nutritious diet, and avoiding harmful fats like oxidized omega-6 oils are crucial for maintaining vascular health and reducing inflammation. Individuals with good metabolic health, who effectively manage their glucose and diet, are at a reduced risk of experiencing the adverse effects associated with high levels of lipoproteins.
Key Indicators of Cardiovascular Health. Key indicators of a healthy heart include efficient pumping capability, allowing the heart to circulate blood effectively throughout the body without undue stress. Optimal blood pressure is essential to prevent damage to the heart and arteries, reducing the risk of heart disease. Additionally, maintaining flexible, plaque-free arteries is crucial as they need to adapt to changes in blood flow, pressure, and volume effectively.
Citations
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.