Rapamycin
The most powerful tool to stop the acceleration of aging caused by mTOR dysfunction and cellular senescence.
Mikhail Blagosklonny's theory of cellular hyperfunction has shifted our understanding of aging by proposing that it's not a result of cellular decline or damage accumulation, but rather an overactive state of cellular metabolism. This idea challenges conventional wisdom and suggests that aging is a reversible phenomenon that can potentially be slowed down or even reversed. This shift in understanding has significant implications for how we approach the aging process.
rapamycin
hyperfunction
11 mins
By: Daniel Tawfik, Jacob Rose
For centuries, scientists and philosophers have been perplexed by the aging process and the ultimate question of why we are mortal. Traditionally, we have believed that aging results from wear and tear and the gradual loss of cellular function. This understanding has been rooted in the idea that living organisms have a limited ability to repair themselves, leading to the accumulation of damage over time.
However, recent research has proposed an entirely different perspective, challenging the notion that aging results from the loss of cellular function. According to this counterintuitive theory, known as cellular hyperfunctionality, age-related diseases are caused by excessive cellular activity, not by a loss of function or damage to tissues. This shift in understanding has significant implications for how we approach the aging process and has captured the attention of longevity scientists.
The theory of hyperfunction in aging is a phenomenon popularized by Dr. Mikhail Blagosklonny; it aims to explain much of the aging process and the success of drugs like rapamycin through the lens of cellular overactivity.
Generally speaking, diseases of aging are characterized by cellular 'hyper-functions,' not the loss of cellular function or 'wear and tear' of tissues.
Blagosklonny outlines three hyperfunctional features to describe the morphology and pathology of a dysfunctional cell. These include hyperplasia, hypertrophy, and hyperfunctionality:
Hyperplasia
is a form of cellular proliferation that is characterized by an increase in the number of cells within an organ or tissue. Senescent cells excessively excrete mitogens, which stimulate cell replication of adjacent cells, which can be pathological, as in the case of cancer or benign tumors.
Hypertrophy
, on the other hand, is an increase in the size of individual cells, leading to an overall increase in the size of the organ or tissue. However, if it persists for an extended period or becomes excessive, it can result in cellular dysfunction, tissue damage, or disease.
Hyperfunctionality
refers to the increased activity of cells or organs beyond what is normal or necessary. Cellular hyperfunctionality can occur due to several factors, including excessive stimulation by hormones or growth factors or abnormal signaling pathways. Hyperfunctionality can result in cellular damage, dysfunction, or disease.
Cell hypertrophy, hyper-function, and hyperplasia drive the acceleration of tissue dysfunction and aging in humans. This counterintuitive understanding of aging as a phenomenon of cellular overactivity has profound implications for how we think about deaccelerating the aging process.
Blagosklonny postulates that the activity level required for cellular growth and proliferation is at the heart of many age-related diseases. As we age, our cells cannot effectively halt or slow the functions needed to grow from children to adults.
He describes this hyperfunction most effectively when comparing it to driving a car. As we grow from children to adults, we spend our life picking up speed, and at some point, though, cellular activity needs to slow down the highway speeds of uninhibited growth.
Our cells have programs or molecular brakes, allowing them to rest and slow down. One form of programmed rest is known as quiescence. Quiescent cells are blocked from dividing and become metabolically inactive. One of the most crucial aspects of quiescence cells is their ability to reactivate and reenter the cell cycle, thereby gracefully traversing both highways and neighborhoods.
When we age, our bodies have a tough time slowing down, however. Instead of a leisurely Sunday drive in an aging body, our hyperactive cells haphazardly careen through neighborhoods at highway speeds, causing damage as they go.
This inappropriate cellular hyperactivity eventually leads to age-related diseases like cancer and osteoporosis. The ability to rest when rest is required and activate when damage occurs, or nutrients are plentiful is a robust program when our cells are young. As we age, however, this self-regulation of healthy growth gets complicated, especially with the introduction of senescent cells.
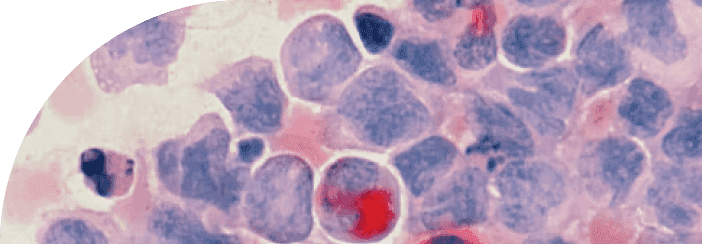
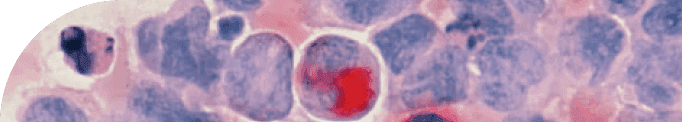
As we age, senescent cells become increasingly prevalent in our bodies. Cellular senescence is a natural process when cells enter a state of permanent growth arrest, meaning they stop dividing and replicating.
Senescence is triggered when a cell becomes damaged. When cells experience excessive stress or damage, they can become senescent, preventing further damage from proliferating and leading to tumorigenesis. We need senescence as a cellular program to stop the spread of cell damage when a cell replicates.
Although these cells have permanently exited the cell cycle and cannot replicate, they remain highly metabolically active, releasing pro-inflammatory and growth-promoting molecules that can contribute to developing various age-related diseases.
The fact that senescent cells cannot replicate impacts their size, activity, and pathology.
When a healthy cell is exposed to growth stimuli, it can balance out its growth by dividing. Senescent cells cannot share the burden of growth with other cells by simply dividing. Instead, when senescent cells are exposed to growth signals, they become very large, hyper-mitogenic, releasing molecules that stimulate the proliferation of adjacent cells, and are resistant to programmed cell death.
Senescent cells also become highly inflammatory—a feature of their hyperfunctionality. They excrete a witch's brew of inflammatory molecules and growth factors known as the senescence-associated secretory phenotype (SASP). The SASP is a complex set of signaling molecules released by senescent cells, which can damage and stimulate nearby cells to divide and grow.
As a result, senescent cells are effectively "stuck" in a state of high activity, with both the gas pedal and the brakes pressed to the floor. The only way for senescent cells to be cleared from the body is through the action of nearby immune cells, which can recognize and remove them. As we age, however, the proportion of senescent cells increases as they become harder to remove—this has tremendous implications for the acceleration of aging.
Viewing cell senescence as a state of continuous growth stimulation in the absence of cell division helps to connect the process of cellular aging to the broader phenomenon of organismal aging.
Many people associate age-related diseases with the terminal loss of cellular function, the opposite of hyperactivity. Cellular senescence is often perceived as a manifestation of functional decline or wear-and-tear, which can lead to the accumulation of cellular damage that exceeds the body's self-repair mechanisms. As a result, many researchers and anti-aging advocates have focused on developing strategies that compensate for the losses and declines associated with aging and support cellular repair and regeneration.
Although it may seem counterintuitive, the loss of function we associate with aging is a secondary effect of cellular hyperactivity and the spreading of cellular dysfunction throughout the tissue it comprises.
One of the most dramatic examples is a heart attack, where the loss of function is the heart's ability to pump blood efficiently. However, we now understand that the heart loses its ability to beat through the action of hypertrophic, enlarged, smooth muscle cells that increase the thickness of the walls in the heart. It is the hyperfunction of the smooth muscle cells that leads to the loss of function of the tissue.
Cellular hyperfunction, hyperplasia, and hypertrophy of smooth muscle cells lead to atherosclerosis and hypertension, ultimately leading to strokes and myocardial function.
Blagosklonny connects nearly every age-related disease to hyperactivity rather than loss of cellular output.
In osteoporosis, osteoclasts become outsized and overactive leading to the resorption of bone tissue.
Alzheimer's disease and other neurodegenerative disorders exhibit a classic hyperfunction behavior. In Alzheimer's disease, mTOR overactivation leads to excess Tau protein excretion, leading to neurodegeneration of the tissue.
Both enlarged prostate and male pattern baldness (androgenic alopecia) are caused by excessive androgen stimulation.
As we age, the hyperactivity of keratinocytes can lead to the formation of wrinkles. Specifically, the overproduction of keratinocytes can lead to an excess of keratin, which can cause the skin to become thicker and less elastic. This reduced elasticity can make the skin more prone to developing wrinkles and fine lines.
These are just a few examples of cellular hyper-functions damaging the health of the tissue it comprises. With this understanding of hyperfunctionality, it would be most effective to halt this initial hyperfunction before the molecular streets become damaged to the point where they cannot be driven on, causing a terminal loss of tissue function.
So, what do our cells' molecular brakes look like, and in what contexts are they engaged?
First and foremost, our cells pump the brakes when there aren't enough nutrients around. If there isn't gas available, the car won't move. Both in the lab and in human life, this can be accomplished with caloric restriction.
Scientists have long known that for a cell to enter into a growth phase, it requires sufficient energy to fuel growth. However, what happens when a cell is faced with an energy deficit? Recent research has shed light on the cellular process known as autophagy, which allows cells to survive under conditions of low energy availability.
Autophagy is the process by which cells recycle their cellular debris, misfolded proteins, and organelles to use as energy. During autophagy, the cell breaks down these unwanted or damaged components into small molecules that can be used to generate ATP, the primary energy source for cells.
This process provides the cell with the energy it needs to survive and helps maintain healthy cell function by clearing out unwanted or potentially harmful materials.
Autophagy can help mitigate the harmful effects of senescent cells by removing damaged or excess cellular components that may contribute to the senescent cell's pro-inflammatory and mitogenic activity. Additionally, autophagy can help promote senescent cell clearance, allowing the body to remove these potentially harmful cells more effectively.
The data is abundant that caloric restriction has a positive association with lifespan. However, despite its potential benefits, caloric restriction can be impractical and challenging to maintain consistently.
Alternatively, there are pharmacological brakes that stifle the cellular growth engine, mTOR.
mTOR (mammalian target of rapamycin) is a protein kinase that plays a crucial role in regulating cell growth, metabolism, and other cellular processes.
You can think of mTOR as the air-traffic controller for cellular growth. When cells receive signals that indicate an abundance of nutrients or growth factors, mTOR becomes activated and stimulates cellular protein synthesis and cell growth. This activation of mTOR promotes cell growth and division, which is essential for tissue repair and growth in developing organisms.
However, when nutrients are scarce, mTOR activity decreases, which triggers the cell's autophagy machinery to assemble to break down and recycle its components to generate energy and nutrients. By initiating autophagy, the cell can maintain its energy balance and survive during times of nutrient scarcity.
Chronic overactivation of mTOR is at the foundation of many age-related diseases. As we get older, mTOR may stay active all the time—opening the door to out-of-control cell growth that can lead to cancer and closing the door on cell repair. It is a driver of cell hypertrophy, hyper-function, and hyperplasia, leading to the decline of healthy tissue. In total, the overactivity of the mTOR pathway is involved in cell senescence, organism aging, and diseases of aging.
Lowering mTOR activity represents a broadly applicable treatment to reduce cellular hyper-functions and the following decline of tissue function.
Rapamycin is a molecule known to inhibit mTOR activity, and it has been studied extensively for its potential to delay aging and prevent age-related diseases. It is one of the most promising tools to combat senescence and toxic cellular hyper-functions.
By targeting and suppressing the mTOR pathway, rapamycin effectively mitigates the release of detrimental molecules from senescent cells. This not only safeguards neighboring tissues from potential harm, but also encourages the elimination of these aging cells through the natural process of autophagy. Consequently, rapamycin plays a crucial role in decelerating the accumulation of cellular damage and reducing the overall population of senescent cells, thereby mitigating their harmful effects on our bodies.
The inhibition of mTOR represents a promising approach for deaccelerating aging by reducing cellular hyperfunction, increasing autophagy, and decreasing senescent cell pathology. Using molecules like rapamycin, we can utilize mTOR inhibition to hinder cancer progression, deter overactive osteoclasts, and neuter increased secretion from senescent cells.
As Blagosklonny might say, like aging, driving a car without proper brakes can be a scary endeavor, but we believe with the advancements in research and extra help from medicines like rapamycin, there are more options than ever to make the elderly neighborhood streets safe from hyperactive cells and deaccelerate the aging process.
Citations
Latest Longevity Research Straight to your Inbox
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.
Sign up for The Longevity Blueprint, a weekly newsletter from Healthspan analyzing the latest longevity research.